The Applications of CRISPR in Optimising Animal Models for Human Disease Research

Animal models for human disease benefit clinical trials in expediting the speed of research, with gene editing helping to make these models more accurate in their predictive capabilities.
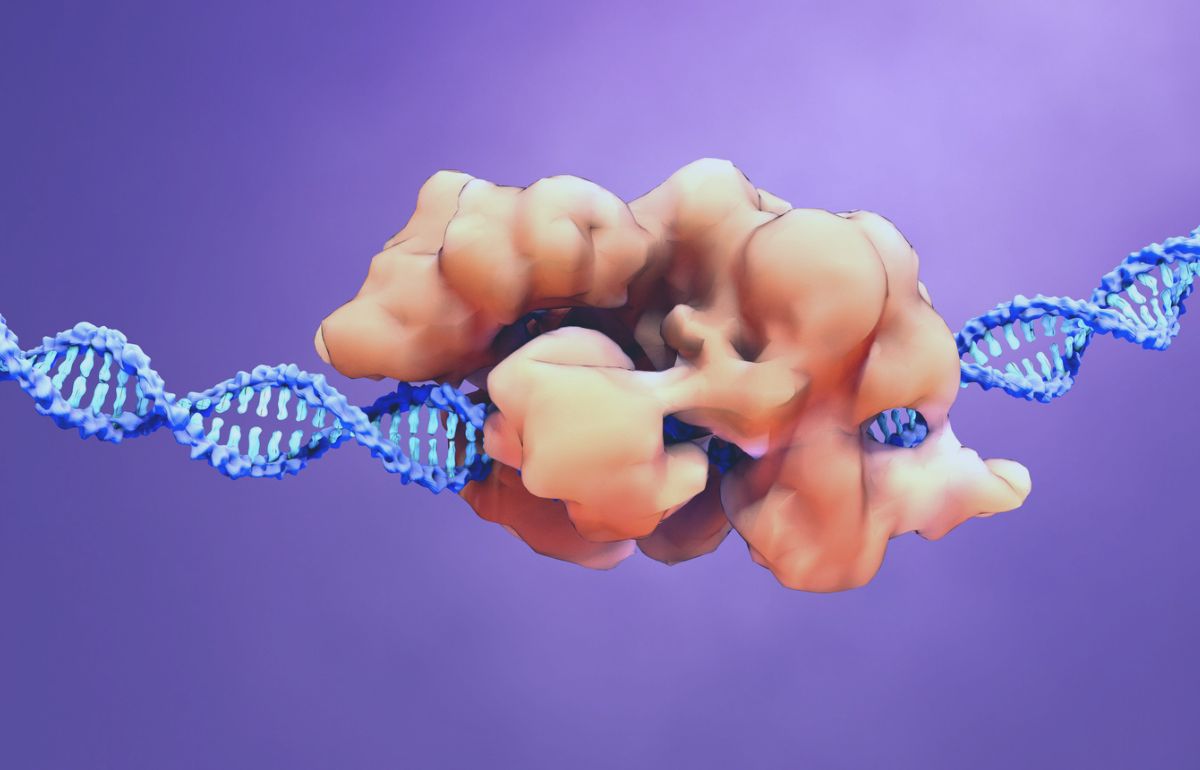
The introduction of the CRISPR (clustered regularly interspaced short palindromic repeats) system has enabled a faster and cheaper production method for animal models compared with traditional methods of gene-targeting using embryonic stem cells.
Despite having only been introduced to the world ten years ago, CRISPR gene editing has been successfully used in animals to manipulate their genomes and recreate the properties of the human interior.
By inverting genomic regions in animal models for human disease, scientists can produce more predictive cell-based models and identify new drug targets in a quicker, more cost-effective way.
Since 2013, various animal models of disease have been generated using the CRISPR-Cas9 system.
Genetic dependences previously undetectable through in vitro screening efforts have been exposed by the application of CRISPR screening in organoid models and whole animal models.
Modifications for modelling complex human diseases that formerly took months or even years to achieve can now be achieved in weeks, and new ground is continually being broken in the field.
In early November 2023, a research team at the Guangzhou Institute of Biomedicine and Health, Chinese Academy of Sciences created a monkey chimera with two sets of DNA.
The animal was created by combining stem cells from a long-tailed macaque with a genetically distinct embryo from the same species.
The proof-of-concept study noted the monkey was "substantially chimeric", containing a varying but relatively high ratio of cells that grew out of chimeric stem cells throughout its body.
One particularly useful observation was that the monkey chimera had a big contribution of stem cells to the brain, suggesting the approach could be valuable for modelling neurodegenerative diseases further down the line.
Applications of CRISPR and Animal Models for Human Disease
Animal models generated through CRISPR technology have been crucial in the discovery of new medicines.
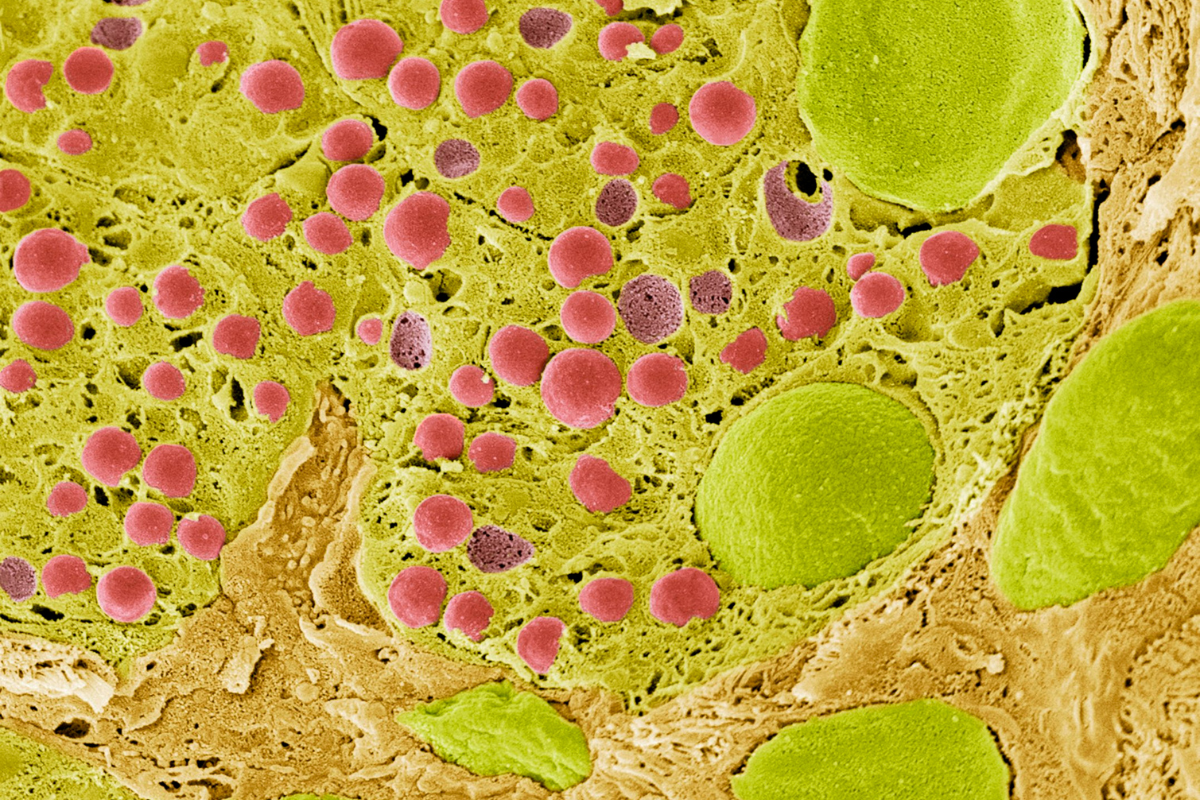
The approach is particularly popular in mouse models, generating highly customised mice and rats whose DNA has been altered to reflect a humanised immune system.
This enables precision modelling in research, as well as target validation and efficacy assessments.
Prior to the introduction of CRISPR technology in animal models, it could take up to 18 months to produce test animals: this now takes approximately half the time, improving cost-effective approaches in comparison to alternative preclinical animal models.
Predicting treatment efficacy is another priority when planning for costly and time-consuming trials.
As animal models can emulate human physiology, they can help to generate reliable data that shows the efficacy and safety of treatment.
To evaluate and ensure translation between humans and animal models, CRISPR streamlines the creation of single nucleotide polymorphisms (SNPs), which are the most abundant source of genetic variation in the human genome.
Safety in Drug Development
Safety is imperative in the drug development process: before studies can translate to human targets, the clinical risk of a potential new treatment must be predicted.
Data derived from animal models instils trust in the technique and the safety of a particular approach.
While the clinical trials industry has witnessed a 5.8% annual growth year on year, the growth of sites is not keeping pace.
Integration of animal models for human disease into clinical trial pipelines can help to ensure a study is faster and move cohesive.
Statistically, only one in ten drugs make it through clinical trials, with the pricetag on bringing a drug to market sitting at an average of USD $985 million.
With hundreds of millions of dollars on the line, optimising revenue in clinical trials is crucial: animal models benefit clinical trials by expediting speed and accuracy.
Based on research and results observed in these models, companies can proceed to the next stage of a particular approach if the data is favourable.
There are limitations to the utility of CRISPR in the incidence of off-target effects of difficulties in creating more complex genome modifications.
Still, CRISPR-Cas9 promises to advance medical applications in treating rare disease, treating - or even potentially curing - illnesses such as cardiovascular diseases and rare inherited blood disorders.
Get your regular dose of industry news and announcements here, or head over to our Omics portal to catch up with the latest advances in tumour analysis. To learn more about our upcoming NextGen Omics US conference in Boston, click here to download an agenda or register your interest.