Chronic Stress Found to Worsen Gut Inflammation

Chronic stress is known to worsen gut inflammation resulting from certain bowel diseases such as inflammatory bowel disease (IBD).
New research from the University of Pennsylvania has now suggested a reason why, outlining a pathway that starts with chemical cues in the brain and ends with immune cells in the gut.
As well as explaining how chronic stress can trigger physical diseases, the study also implies that managing stress levels may have a profound influence over the effectiveness of treatments for IBD.
While the suggestion runs contrary to conventional medical treatment that have purportedly neglected the psychological state of a patient as a major driver of responses to treatment, the findings have the potential to reinforce healthcare provision for those suffering bowel disease.
A research team from the University of Pennsylvania, led by Christoph Thaiss of the Penn Institute for Technology, used a mouse model to investigate mechanisms underlying the impact of psychological stress on intestinal inflammation.
RNA sequencing of colonic tissue derived from the models revealed pronounced changes in gene expression induced by psychological stress.
As a real-world example of how this works, stressful events such as bereavements or break-ups can precede IBD flare-ups.
After a surge of dress, the brain sends signals to the adrenal glands, which release chemicals called glucocorticoids into the rest of the body.
Monitoring Chronic Stress and Signalling in Relation to IBD
Initially, researchers considered the idea that glucocorticoids act directly on immune cells, which respond by releasing molecules that cause inflammation.
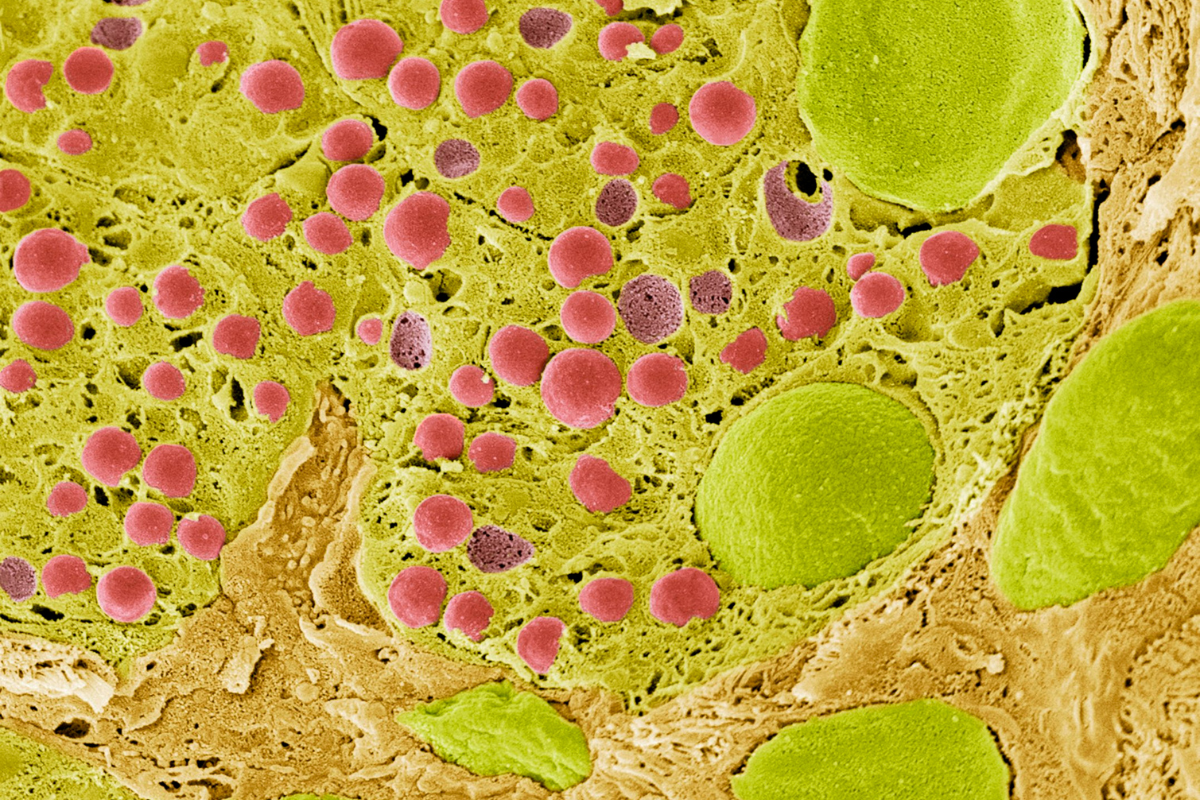
However, it transpired that a layer exists in between: working in mice, Thaiss and his team found that glucocorticoids act instead on neurons in the gut.
After being activated by glucocorticoids, some glial cells release molecules that trigger immune cells.
In turn, those immune cells release molecules that would normally be used to fight off pathogens, but here end up causing painful bowel inflammation.
Researchers were surprised to find that glucocorticoids cause gut inflammation, as these compounds are sometimes used to treat IBD.
- Celebrating the Achievements of Barbara McClintock
- The Wonders of Synthetic Biology: In Conversation with Martin Hanczyc
- Spatial Profiling, Analytical Approaches, and New Transcriptomic Technologies
While this is an apparent paradox, it can be explained by the short timeframe in which such treatments are used.
Although quick bursts of glucocorticoids function in an anti-inflammatory fashion, when stress becomes chronic, the system completely shifts, with glucocorticoids taking on a pro-inflammatory role.
These findings suggest that the brain’s ability to drive inflammation in far-flung organs appears to be much stronger than initially thought.
A key takeaway is that stress management techniques delivered in tandem with IBD drugs could be more effective than drugs alone in dealing with the condition.
Get your weekly dose of industry news and announcements here, or head over to our Omics portal to catch up with the latest advances in spatial analysis and next-gen sequencing.