Understanding and Overcoming the Immunosuppressive TME
The Impact of the Tumour Microenvironment on CAR T Efficacy
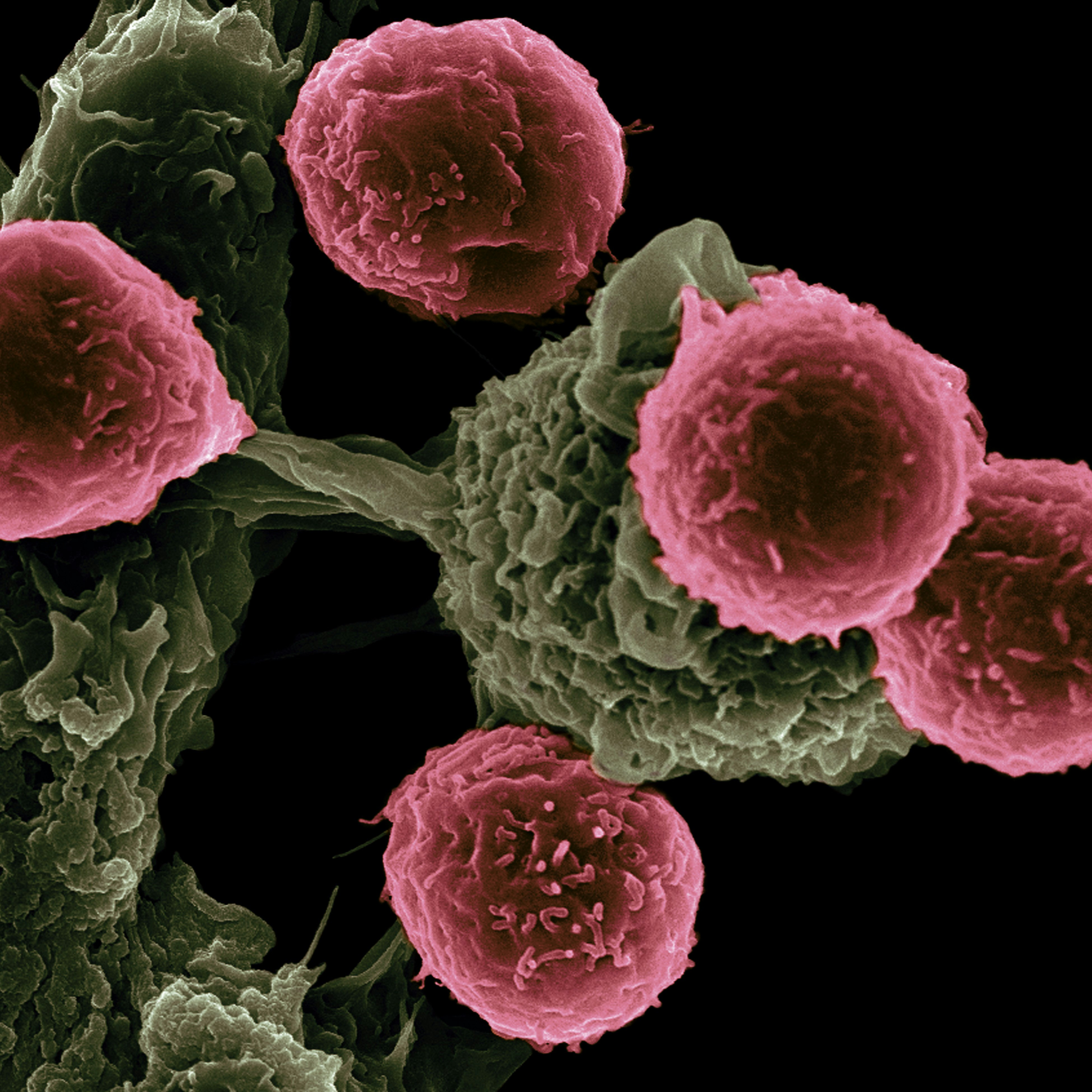
The immunosuppressive tumour microenvironment (TME) poses significant challenges to the efficacy of CAR T therapy in several interconnected ways. Primarily, it creates a hostile environment for CAR T cells, which are engineered to attack cancer cells. The TME is rich in inhibitory molecules like PD-L1, TGF-β, and IL-10, which can suppress the immune response. These molecules directly impact the activity and proliferation of CAR T cells, reducing their effectiveness in targeting and destroying cancer cells.
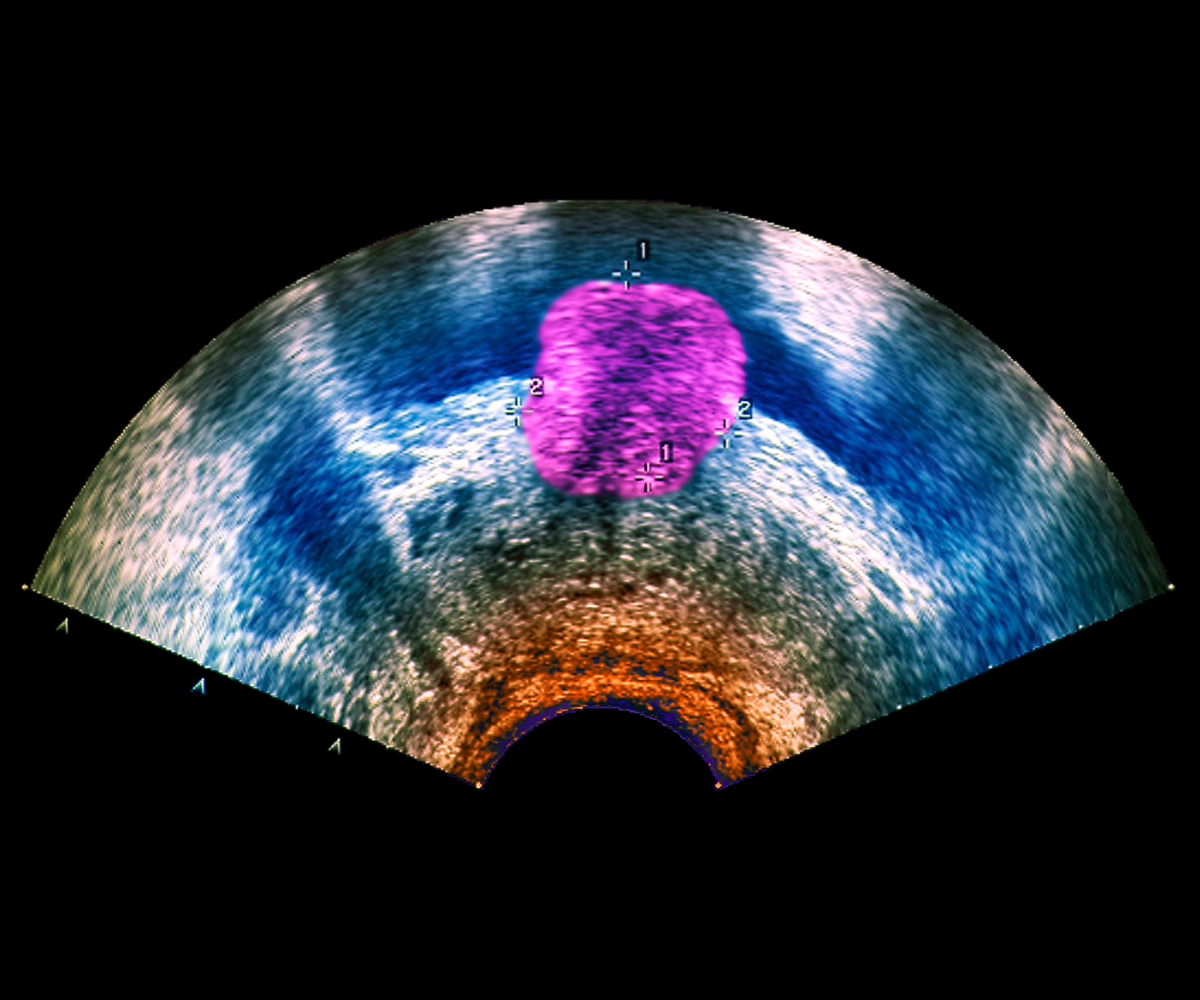
The physical structure of solid tumours presents another hurdle; the dense extracellular matrix and abnormal vasculature of these tumours can impede CAR T cell infiltration, making it difficult for these cells to reach and attack the cancer cells effectively. This physical barrier often leads to a reduced number of CAR T cells in the tumour site, further diminishing the therapy’s efficacy.
The TME is characterized by a complex network of different cell types, including regulatory T cells (Tregs), myeloid-derived suppressor cells (MDSCs), and cancer-associated fibroblasts (CAFs). These cells can further contribute to the immunosuppressive environment. For instance, Tregs and MDSCs can inhibit the immune response against cancer cells, including the activity of CAR T cells.
The metabolic competition in the TME also plays a role; the rapid growth of cancer cells often leads to depleted nutrients and oxygen in the environment, creating a state of hypoxia. This can impair CAR T cell function and survival, as these cells require adequate metabolic support to maintain their anti-tumour activities.
Lastly, the TME can induce phenotypic changes in CAR T cells, such as exhaustion. Continuous exposure to cancer antigens and the hostile TME can lead to the expression of exhaustion markers on CAR T cells, reducing their potency and longevity. Overall, the immunosuppressive TME represents a significant obstacle to the success of CAR T therapy, necessitating ongoing research and development of strategies to overcome these challenges.
Breaking Barriers: Emerging Innovations in CAR T Therapy Resistance
Recent advancements in overcoming resistance to CAR T therapy have been diverse and innovative, reflecting the complexity of this challenge. Researchers have been focusing on several strategies to enhance the efficacy of CAR T cells against resistant tumours.
One key area of advancement is the development of next-generation CAR T cells. These are engineered to be more resilient in the face of the immunosuppressive tumour microenvironment. For example, some are designed to secrete cytokines that can counteract the suppressive effects of the tumour, or they are modified to be resistant to inhibitory molecules found in the tumour microenvironment.
Another significant development is the targeting of multiple antigens. Traditional CAR T therapies target a single antigen on cancer cells, but tumours can evade this by losing or altering that antigen. By targeting multiple antigens simultaneously, the therapy can reduce the likelihood of the cancer cells escaping detection and destruction.
Additionally, researchers are exploring the combination of CAR T therapy with other treatments, such as immune checkpoint inhibitors. These inhibitors can block the proteins used by cancer cells to suppress the immune system, potentially making CAR T cells more effective.
The use of “armoured” CAR T cells is also a notable advancement. These CAR T cells are engineered to express additional proteins that can help them overcome the immunosuppressive signals in the tumour microenvironment. This armour can make the CAR T cells more robust and enduring in hostile environments.
There is also ongoing research in improving CAR T cell trafficking and penetration into solid tumours. Improvements in the ability of CAR T cells to navigate to and infiltrate solid tumours could significantly enhance their effectiveness.
Finally, there is a growing interest in understanding and reversing CAR T cell exhaustion. Exhaustion occurs when CAR T cells become less effective over time due to chronic exposure to their target antigen. Research in this area focuses on identifying the mechanisms behind exhaustion and finding ways to rejuvenate or replace exhausted CAR T cells.
These advancements represent a multifaceted approach to overcoming the limitations of current CAR T therapies, promising more effective treatments for patients who currently have limited options.
The Frontier of CAR T: Next-Gen Solutions to Tumour Microenvironment Challenges
Next-generation CAR T therapies are addressing the challenges posed by the tumour microenvironment (TME) through several innovative approaches. One of the primary methods involves engineering CAR T cells that are more resilient to the suppressive factors present in the TME. This can include making them resistant to certain inhibitory molecules or enabling them to secrete cytokines that counteract the immunosuppressive environment. By doing so, these enhanced CAR T cells can maintain their activity and effectiveness even in the hostile milieu of the tumour.
Another focus is on improving the trafficking and infiltration capabilities of CAR T cells. In solid tumours, the dense extracellular matrix and abnormal vasculature often impede the entry and movement of CAR T cells. By modifying these cells to navigate this complex structure more effectively, they can reach and attack cancer cells more efficiently.
There’s also an emphasis on targeting multiple antigens. The heterogeneity of antigens expressed by tumour cells in the TME means that targeting a single antigen may not be sufficient. Next-generation CAR T cells are being designed to recognize and attack multiple antigens, reducing the likelihood of tumour escape due to antigen loss or mutation.
Combination therapies represent another strategic approach. By pairing CAR T therapies with other treatments, such as immune checkpoint inhibitors, the overall efficacy can be enhanced. This combination can help modulate the TME, making it more conducive to CAR T cell activity.
Moreover, addressing the issue of CAR T cell exhaustion is critical. Continuous exposure to antigens and the suppressive TME can lead to a decrease in CAR T cell functionality over time. Research is ongoing to understand this phenomenon better and to develop strategies to rejuvenate exhausted CAR T cells or replace them with fresh, active cells.
Research is also focusing on personalizing CAR T therapies based on individual TME characteristics. This personalized approach can involve tailoring the CAR T cells to the specific immunosuppressive factors and antigen profiles present in a patient’s tumour, potentially leading to more effective and durable responses.
These advancements collectively represent a comprehensive effort to overcome the unique challenges posed by the TME, aiming to enhance the efficacy of CAR T therapies in treating a variety of cancers.
Revolutionizing Solid Tumour Treatment: New Horizons in CAR T Therapy Strategies
Enhancing CAR T therapy in solid tumours involves innovative strategies that address the unique challenges posed by these types of cancers. One of the main focuses has been on improving the ability of CAR T cells to penetrate and survive in the dense and hostile microenvironment of solid tumours.
To tackle the issue of penetration, researchers are developing CAR T cells with enhanced mobility and the ability to navigate through the complex extracellular matrix of solid tumours. These engineered cells can more effectively infiltrate the tumour mass, increasing their contact with cancer cells.
Another strategy involves modifying CAR T cells to resist the immunosuppressive factors within the tumour microenvironment. This can be achieved by engineering them to express certain proteins or cytokines that can counteract the suppressive effects of the environment, or by making them resistant to specific inhibitory molecules present in solid tumours.
Combination therapies are also being explored. Combining CAR T therapy with other treatments, such as immune checkpoint inhibitors, oncolytic viruses, or traditional chemotherapy, can help weaken the tumour and make it more susceptible to CAR T cell attack. This approach can also help modulate the tumour microenvironment to be less hostile to CAR T cells.
Addressing the issue of antigen heterogeneity in solid tumours is another important strategy. Since solid tumours often express a variety of antigens, there’s a risk of the tumour evading treatment if only one antigen is targeted. Developing CAR T cells that target multiple antigens simultaneously can help mitigate this problem and increase the chances of successfully eliminating the tumour.
Lastly, improving the persistence and endurance of CAR T cells in the body is crucial. Researchers are working on ways to enhance the longevity and anti-tumour activity of these cells once they are inside the patient. This includes finding ways to prevent or reverse CAR T cell exhaustion, a state where the cells become less effective over time.
These strategies collectively aim to overcome the specific challenges posed by solid tumours, making CAR T therapy a more viable and effective treatment option for these types of cancers.
Want to read more about new advances in immuno-oncology and ongoing immune therapies? Sign up to our Immuno newsletter to receive leading experts opinions, research and cutting-edge presentations on the latest advancements in cancer immunotherapy, with dedicated sessions on different therapeutic modalities as well as case studies on innovative preclinical and translational tools.