The Therapeutic Modulation of Cytokines with Pierre Ferré, VP of Pre-Clinical Development, Compugen

We sat down with Dr. Pierre Ferré, Vice President of Pre-Clinical Development at Compugen, to discuss their therapeutic, COM503, which was recently presented at the Society for the Immunotherapy of Cancer (SITC) conference.
Dr. Ferré has two decades of experience in all aspects of clinical and non-clinical drug development in oncology and immuno-oncology. Dr. Ferré joined Compugen from Pierre Fabre Pharmaceuticals, France, where he spent most of his career in multiple positions, most recently as Director of Oncology Programs in which he led the development strategy of a portfolio of R&D programs in oncology from initiation and discovery, through preclinical and clinical development.
RELATED:
- Compugen: Exploring New Pathways and Combinations in Immunotherapy
- Cancer Immunotherapy Novel Targets: The Forefront of Immuno-Oncology Research
- European Commission Approves Genmab’s Subcutaneous Bispecific Antibody Tepkinly
Previously, at Pierre Fabre Oncology R&D, he acted as Director, Pharmacokinetics/Pharmacodynamics, overseeing also translational, biomarker-related activities. Before that Dr. Ferré was in charge of oncology preclinical pharmacokinetics. Dr. Ferré holds a PhD in biology, from Toulouse INP (Institut National Polytechnique), and a MSc from Aix-Marseille University and Paris INA-PG (Institut National Agronomique) for his research work conducted in experimental pathophysiology and toxicology.
In recent years, how has the therapeutic modulation of cytokines progressed? What challenges has the field faced through its development?
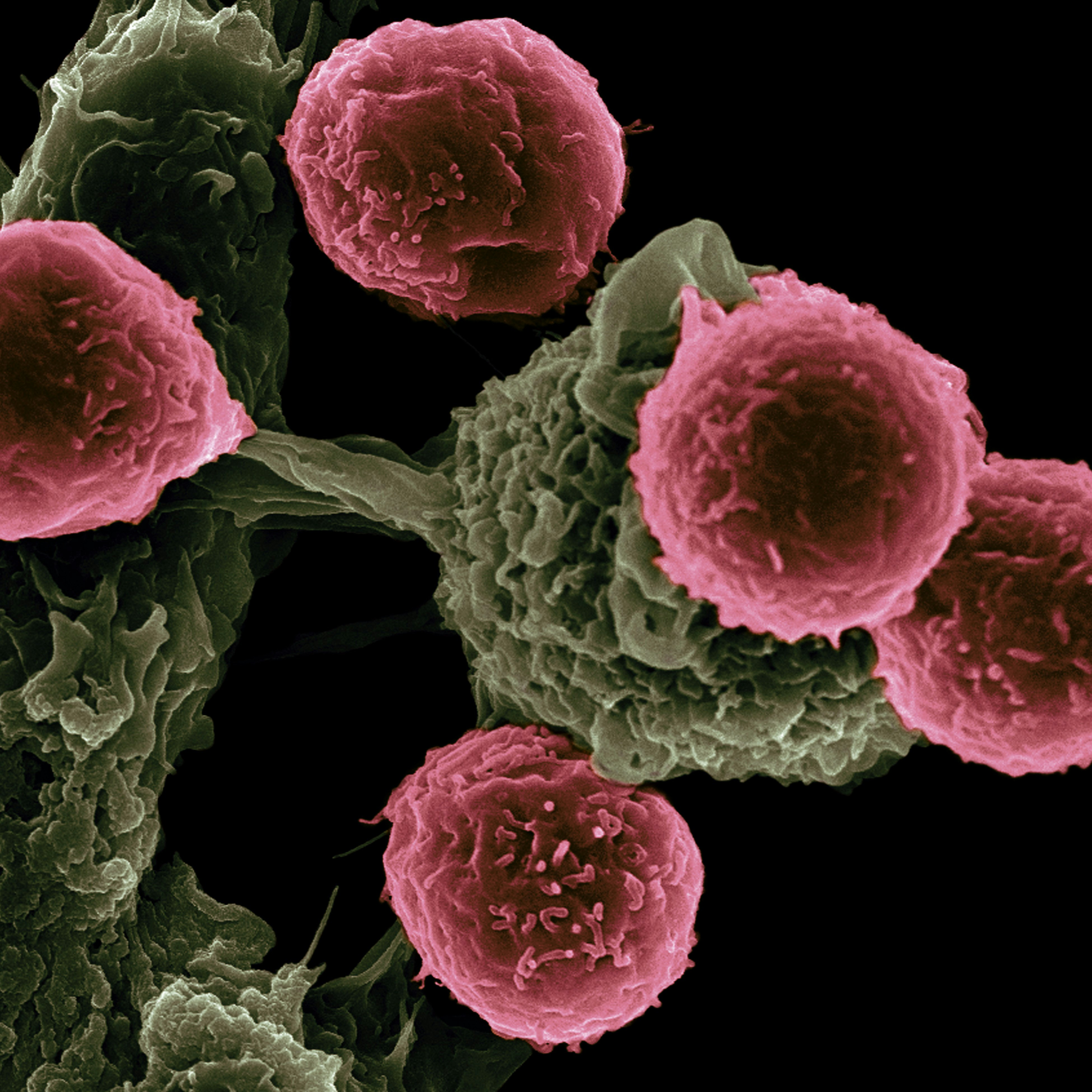
Cytokines are very powerful molecules; many biotechs and pharma, as well as academics, have wanted to use them as drugs because they are very potent activators of the immune system - T cells or NK cells, for instance. And so there have been lots of attempts at fine tuning cytokine therapies.
But since the 90s, when IL-2 and interferon were approved for use in melanoma and renal cancer, there was not much success. We wanted to weigh in, and we found an approach which is a real opportunity to get cytokine therapies working in cancer, which we hope will be transformative for patients. This opportunity is in the interleukin-18 (IL-18), interleukin-18 binding protein (IL-18BP) pathway, which I’ll describe in more detail later.
The reason why cytokines didn’t initially seem like a valuable approach is, we think, because cytokines are very potent in activating T cells and NK cells. So potent that when you give them to patients, they encounter and activate the circulating T cells and NK cells and cause toxicity at a level that would limit their efficacy. Once activated, those cells produce cytokines which in turn activate other cells, which can produce cytokine cascades and storms, something known as cytokine release syndrome. That's the first thing.
The second thing is that the pharmacokinetics of cytokines is not great. They are quickly eliminated from the blood and for that reason, it’s not easy to make them into drugs.
Related to those two factors is that it's very difficult for cytokines to reach sufficient concentrations in the heart of the tumour, where they are needed for anti-tumour activity from the T cells and the NK cells.
COM503's mechanism of action is centred around this immunosuppressive mechanism (“interleukin-18 binding protein and interleukin-18 complex”) for tumour immune-escape that you identified - could you explain this mechanism?
Yes, interleukin-18 is a very special cytokine because it's potent in activating T and NK cells. But Mother Nature, quote-unquote, has this mechanism of binding protein (IL-18BP), which is specific to IL-18 and not seen with other cytokines. Naturally, the tumour microenvironment produces IL-18, but it also produces its IL-18BP, its binding protein, which binds to IL-18 and deactivates it. So IL-18 is still around, but it is blocked from stimulating its receptor.
That's the mechanism that we think we can tackle. As those two molecules, IL-18 and its binding protein, are present in the tumours, we want to let the endogenous IL-18 activate the T and NK cells at the heart of the tumour and do their job.
How did Compugen identify IL-18BP?
At Compugen, we have bioinformatic scientists that are constantly looking for new targets that can be used to kill the tumour. We were interested in genomic and transcriptomic databases from patients’ tumours to understand the mechanism of resistance to immunotherapy that we are trying to tackle. Some patients have a lot of immunosuppressive cells in the tumour microenvironment, so we were interested in that.
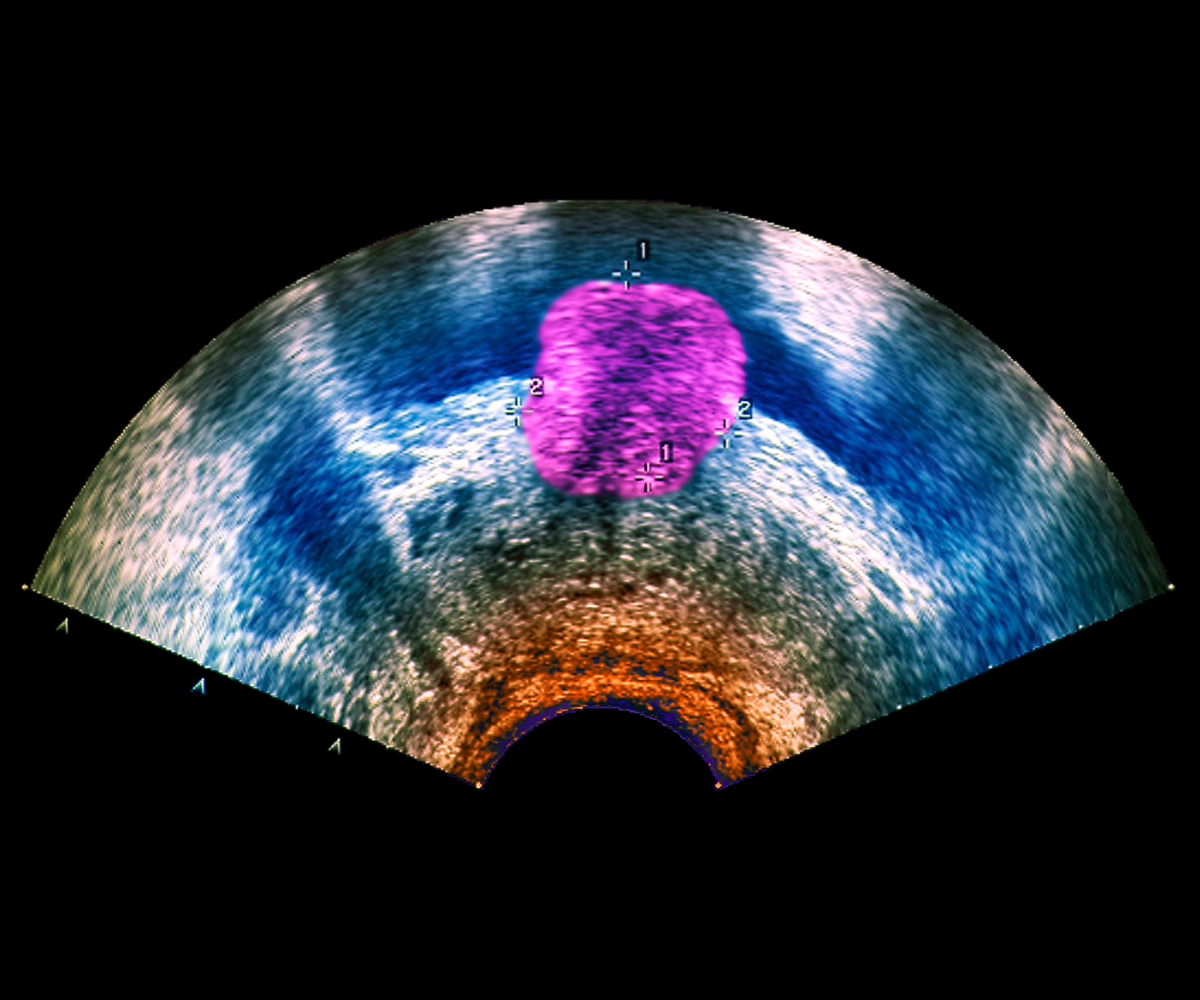
Within those immunosuppressive cells, we discovered that in some tumours, the myeloid cells produce a lot of IL-18BP while the myeloid cells in the peripheral blood mononuclear cells did not. So we were intrigued by that, and that's how we discovered that those tumours which had immunosuppressive myeloid cells, the same cells also produced lots of IL-18BP.
So how does COM503 tackle this mechanism for the treatment of solid tumours?
The interaction between IL-18 and its binding protein (IL-18BP) is very strong as BP is natural inhibitor of IL-18. So, we had to design an antibody that would be able to block that interaction. This antibody needs to have a very high affinity for the binding protein so that it is able to either break the complex of IL-18–IL-18BP, or to sufficiently occupy the binding protein so that IL-18 cannot bind to it.
So, this is how it works: COM503 is a very high affinity antibody, which is administered systemically. Then, once distributed throughout the body and in the tumour, it then binds to IL-18 BP releasing the natural endogenously produced IL-18. Then, IL-18 free from IL-18BP, can activate the T cells and the NK cells locally in the tumour where you need it.
Could you tell me about how the preclinical phase went for COM503?
Compared to other ways of driving IL-18 into the tumour, like having a drug modality that uses IL-18 as a backbone, we designed the preclinical programme based on an antibody. That’s what we know how to do – we have other drugs in the clinic currently which are monoclonal antibodies.
So, it's a therapeutic monoclonal antibody, where CMC production is easy and well documented. Furthermore, it is a human antibody, so the immunogenicity profile should be low compared to other, fancier drug modalities.
The preclinical programme needed to develop our COM503 antibody drug candidate as a drug, which is relatively straightforward nowadays. We also conducted a package of efficacy studies in mice models, where we have seen that, indeed, the antibody blocks IL-18BP and reshapes the tumour microenvironment completely in mice bearing tumours. So, we have great activity and efficacy in mice tumours and the microenvironment is completely changed. We induce T cell activation and proliferation, better myeloid cells that become pro-inflammatory rather than immunosuppressive, and lots of dendritic cells are activated to better educate the immune system.
That’s the data that we have from the mice models. And we also, found that the IL-18–IL-18BP pathway in mice is equivalent to the human pathway, so we can make inferences from the anti-tumour activity that we see in mice.
Apart from mice, we have other pharmacological activity tests that use human cells and human dissociated tumour cells where the activity of COM503 is also exemplified.
We also have all the safety studies that we needed to do in order to prepare for IND-filing. These are standard in vivo studies where COM503 is given at very high doses, and studies using human cells to make sure that we don't have any potential cytokine release in the blood.
Where do you get the human cells that you work with preclinically?
We use fresh tumours that we get from the hospitals we are collaborating with. It's difficult to set up, the logistics from the hospital to the lab needs to be very fast, but we managed to do it. We start by dissociating the tumours gently, because we need to keep the microenvironment the best it can be, and then we spike that with COM503 and incubate it. Then we look in the medium to see that the T cells are activated and killing some of the tumour cells that are present.
It’s a very interesting model. The model’s function is exemplified by what we see in mice and also what we see in these real human tumours. Here we move away from in silico modelling: it’s not a clinical trial, but we put the drug directly in the tumour to see its mechanism of action, and we're quite happy with the results we have so far.
What stage is COM503 currently at, and what lies ahead for it?
The preclinical development is ongoing. In its development, pharmacology, safety, and drug production should be ready for the for the clinic soon. In terms of timeline, we think we will file as an investigational new drug (IND) next year, and we are really gearing up to that at the moment.
The communication that we had at SITC gave us more strength and enthusiasm to get COM503 ready and accessible to the patients. We were glad that our abstract was selected by the Scientific Committee at SITC, as a poster and oral communication.
People were coming by the poster the day after the oral session and asking more questions; being very enthusiastic about what we described. They saw that Compugen was advancing a unique opportunity to use an antibody to reactivate the natural IL-18 which is already in the tumour without affecting the periphery. The point that makes the programme attractive is that all of that happens already in the tumour and not much or not at all in the periphery of the mice.
So we had enthusiasm from some of the key academic leaders of the immuno-oncology field, but also from other biotechs working on IL-18, working on drugs that may be combined with IL-18 enabling molecules also, and from pharma companies that were interested in the programme.
Regarding the other competing programme we came across during the oral communication session: this one takes a completely different angle and is already in the clinic. They are using an engineered IL-18, where they modified its sequence to include a mutation that makes it unable to bind to the IL-18 binding protein, while still retaining its capacity to stimulate the T cells and NK cells.
This is a nice idea, to overcome the binding protein, but you have to administer the drug to the patients to achieve systemic circulation. This means that the molecule encounters the T cells and NK cells first in the periphery of the blood before reaching the tumour, potentially leading to safety issues. So, even though the idea is attractive, it will probably be difficult to manage in the clinic, which is what we’ve seen with other cytokines in the past. The good thing is that it reactivates the interest in cytokines within the community, which also brings attention to our programme.
But our programme is completely different. We use an antibody with all the properties that make a good drug: like ease of production and very good pharmacokinetic properties because an antibody stays in the circulation for weeks. And with the opportunity of IL-18BP being localised in the tumour, we think that COM503’s effect will only manifest when the antibody reaches a tumour and not before.
See the upcoming events in Oxford Global’s Immuno series here - including our upcoming conference, Targets & Cell Types in Immuno-Oncology Europe.
Get your weekly dose of industry news?here?and keep up to date with the latest?‘Industry Spotlight’ posts.?For other Immuno content, please visit the?Immuno Content Portal.