Express Your Cells: Enhancing T Cell Function with Small Molecule HPK1 Inhibitors
Edited by Tom Cohen
Preclinical Immuno-Oncology: Online was pleased to welcome Dirk Brockstedt, Chief Scientific Officer of RAPT Therapeutics in May 2022. Brockstedt gave the final presentation of the online conference titled: T Cell Based Therapies: Enhancing T Cell Function with Small Molecule HPK1 Inhibitors.
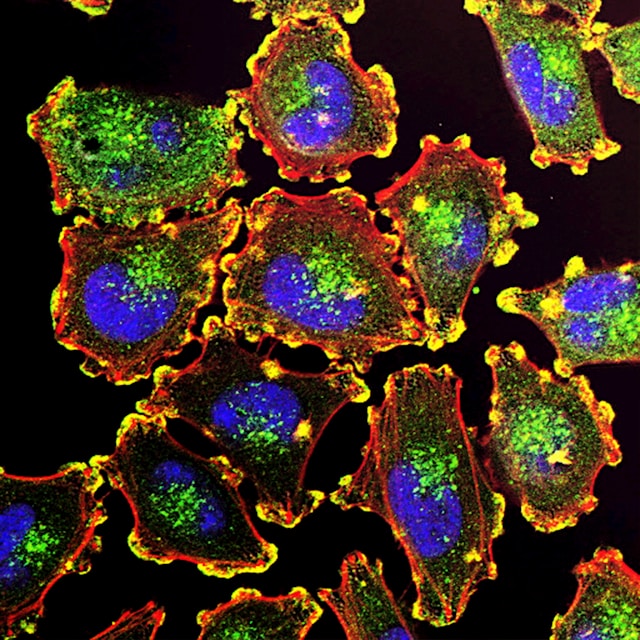
Brockstedt began his talk by explaining that the key effector cells in the tumour microenvironment are T cells, including CD8+ T and Th1 cells. As a result of this, Brockstedt pointed out that the presence of these cells correlates with good prognoses in patients with a diverse array of cancer indications.
Furthermore, the ratio of CD8+ T cells to immuno-suppressive cells (such as Treg cells and M2 macrophages) correlates with clinical outcome, says Brockstedt. This supports the idea that if one could increase the frequency of CD8+ T cells, researchers could effectively achieve better outcome.
Targeting the HPK1 Pathway
Brockstedt’s team at RAPT Therapeutics looked at many ways to enhance T cell function. Notably, they embarked on developing a small molecule drug that targets the HPK1 pathway. “HPK1 is expressed exclusively in immune cells,” Brockstedt explained. The pathway is best understood in the context of T cells, where it has been shown to be a negative regulator of T cell activation.
- Investigating the Core Tenet of Immunotherapy: MHC-I Peptide-Receptor Complexes
- AAV Gene Therapy and CAR T Therapies: Immunogenicity and Immunoassay Development
- Preclinical Strategies for Combination Immunotherapies
The T cell receptor that recognises the MHC-peptide complex leads to the activation and subsequent phosphorylation of HPK1. This then triggers signalling, calcium flux, transcription, and T cell activation. The pathway ultimately leads to the recruitment of E3 ligase which begins degradation and limits further signalling. The team at RAPT as well as others theorised that by blocking HPK1, one could block the recruitment of E3 ligase and subsequent degradation, allowing for more prolonged signalling and T cell activation.
Inhibition of the HPK1 pathway
In T cells
- Enhanced secretion of inflammatory cytokines
- Increased proliferation Increased resistance to PGE2
- Decreased exhaustion
In antigen presenting cells (e.g., dendritic cells)
- Enhanced expression of costimulatory molecules
- Increased levels of proinflammatory cytokines
- Enhanced antigen processing
- Decrease in anti-inflammatory cytokines
Figure 1 – The effects of HPK1 pathway inhibition in T cells and antigen presenting cells. Modified from Brockstedt’s slide.
Small Molecule Drug Development Targeting HPK1
Before designing a small molecule that would target the HPK1 pathway, the team first wanted to validate the target on a genetic level. To do this, they developed a mouse model that phenocopies the abrogation of HPK1 kinase activity. They introduced an amino acid change at amino acid 46, from lysine to methionine, which leads to the abrogation of HPK1 kinase activity. RAPT refers to these as ‘kinase-dead’ mice.
Brockstedt’s team stimulated the CD8+ T cells of the mice, and consequently observed enhanced T cell activation of the kinase-dead mice when compared to wild-type mice. This was also noted in CD4+ T cells, but in both cases, it was not the case when the T cells were stimulated independently of the T cell receptor using PMA/lonomycin.
The team were further able to demonstrate enhanced T cell activation in vivo by using a model where they injected an activating ?-CD3 antibody into the wild-type and kinase-
dead mice. They then measured the cytokines at different points in time (1.5 and 3 hours). The results clearly showed enhanced secretion of IL-2 and IFN-? in serum after 1.5 and 3 hours.
“This nicely translated to enhanced anti-tumour activity,” said Brockstedt. They evaluated two different mouse tumour models (GL261, BF16F10-OVA) and found that tumour growth was reduced in HPK1 kinase-dead mice compared to wild-type mice.
Developing Small Molecule HPK1 Inhibitors
The results of the previous experiments suggested that inhibiting HPK1 would enhance T cell activation. “So, we embarked on the development of a potent and selective oral small molecule inhibitor,” recounted Brockstedt, adding that they used a structure-based drug design method.
Brockstedt focused on one molecule from their series, HPK1-054, which showed excellent biochemical activity at low nanomolar levels. The molecule also presented with good selectivity for HPK1 and cellular potency.
Tests against activated human PBMCs which they had incubated saw a satisfying dose-dependent increase in effector cytokine secretion (IL-2 and IFN-?). “We saw a really nice dose response for both cytokines,” Brockstedt commented.
Next, they assessed the activity of HPK1-054 in CD8+ T cells isolated from wild-type and HPK1 kinase-dead mice. T cells were stimulated in vitro with ?-CD3/?-CD28 for 18 hours before assessing the levels of IFN-? secretion. They saw a dose-dependent increase in the wild-type cells but not cells from the kinase-dead mice which was to be expected, demonstrating good selectivity of their HPK1 inhibitor.
“Next, we wanted to assess how well the compound administered orally could engage the target in vivo,” Brockstedt continued. To do this they administered the compound orally and then injected mice with an anti-CD3 antibody to activate T cells in vivo. The level of SLP76 phosphorylation in CD3+ T cells was determined as a read-out for target engagement. As expected, the control group demonstrated full phosphorylation of SLP76, but critically they observed a dose-dependent decrease in phosphorylation in the groups that were given the compound.
“This inhibition led to significant increases in the induction of antigen-specific CD4 and CD8 T cell responses.” The enhancement of T cell function and immune responses translated to response to tumour development. Importantly, in mouse models of GL261 tumours, it was shown that RAPT’s HPK1 inhibitor given orally was able to result in tumour regressions and, crucially, five out of ten mice ultimately showed tumour clearance. This was compared to the control group which showed steady tumour growth in eight out of ten mice.
Brockstedt concluded the presentation by mentioning how the HPK1 inhibitor synergises well with a variety of immune checkpoint inhibitors. The combination exhibits a decrease in growth rate and even tumour regressions. “RAPT Therapeutics has developed a series of very potent, selective, and orally bioavailable small molecule HPK1 inhibitors,” Brockstedt summarised. RAPT’s inhibitors address an important problem in immunotherapy: ‘the limited and suboptimal priming of CD4+ and CD8+ T cells.’ “We believe that HPK1 inhibition could be one of the modalities that ultimately results in a broad and polyfunctional CD4+ and CD8+ T cell response.”
Gain valuable insights into the approaches impacting the immunotherapy field through 40+ outstanding presentations tackling key discussion points in immuno-oncology, immunology and inflammation. Join Immuno UK: In Person.