The Roadmap of ADC Formulation & Delivery: Achievements and Obstacles

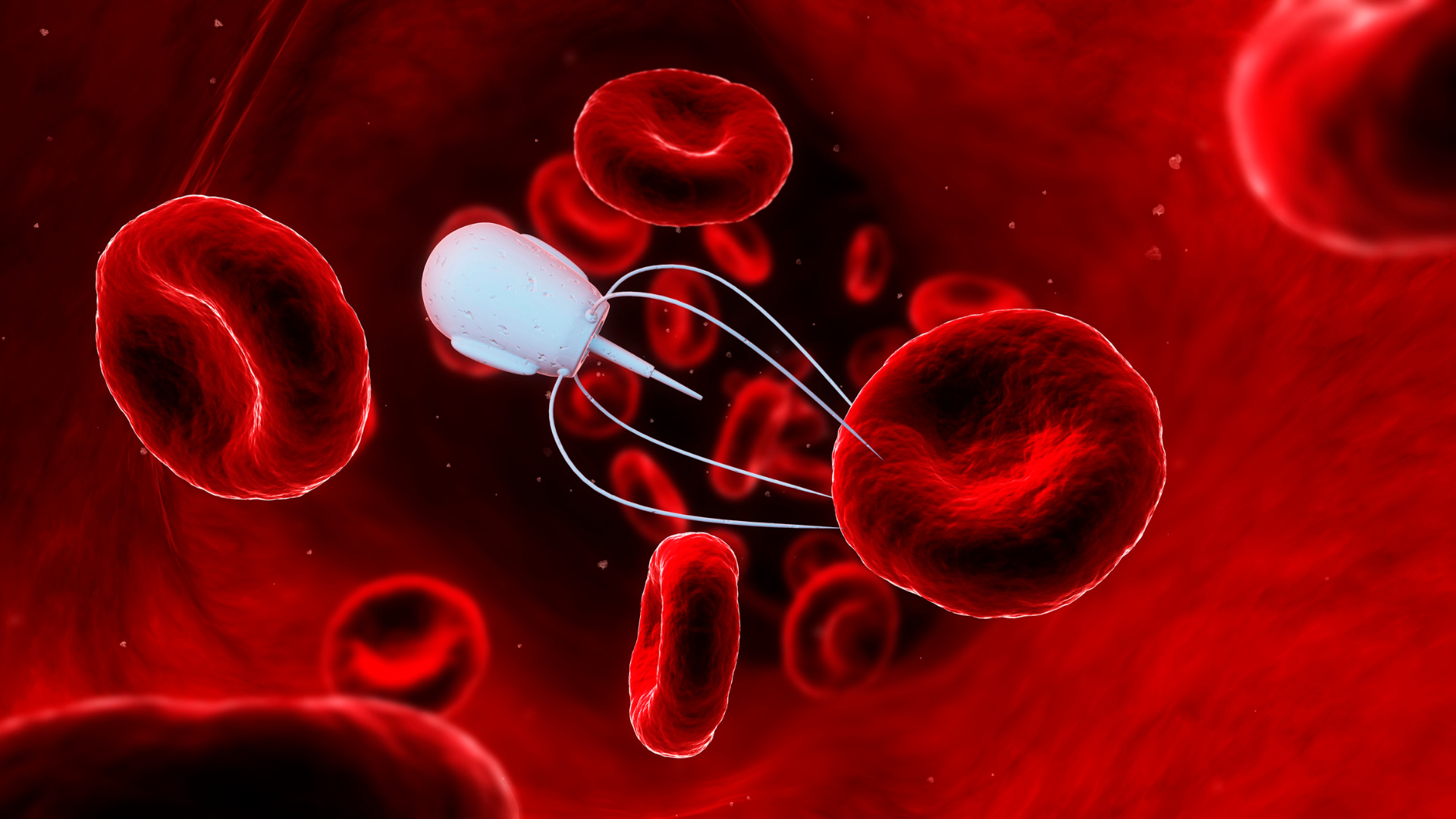
The Roadmap of ADC Formulation & Delivery and the landscape of oncological treatment are undergoing a transformative shift with the development of Antibody-Drug Conjugates (ADCs), a novel class of therapeutics that synergize the specificity of monoclonal antibodies with the potency of cytotoxic agents. This advancement marks a significant stride in the realm of targeted cancer therapy. ADCs represent a fusion of the precision of monoclonal antibodies with the cell-killing power of cytotoxic drugs, aiming to deliver targeted treatment while minimizing side effects.
The recent progress in ADC formulation and delivery is noteworthy, particularly in enhancing their efficacy, reducing toxicity, and improving targeting capabilities pushing the formulation & drug delivery industry even further. The research community is focused on developing ADCs that more accurately target cancer cells, achieved through the discovery and use of new cancer-specific antigens. There's also a significant emphasis on improving linker technology, ensuring that the cytotoxic drug remains attached to the antibody until it reaches the target cell, thereby reducing side effects and preventing premature drug release.
Oxford Global delves deeper into the scientific intricacies of the latest advancements in ADCs, their role in enhancing targeted drug delivery, and the multifaceted challenges encountered in their development.
What are the latest advancements in ADC Formulation & Delivery?
Recent advancements in ADC technology are primarily focused on enhancing the precision of cancer cell targeting. These advancements primarily focus on improving efficacy, reducing toxicity, and enhancing the targeting ability of these therapeutic agents thereby minimizing collateral damage to healthy cells.
This is achieved through the identification of novel tumor-specific antigens, such as HER2 in breast cancer, where drugs like Trastuzumab emtansine (Kadcyla) have shown promising results. The evolution of linker technology is pivotal in this respect. Modern ADCs employ linkers that are stable in the bloodstream yet release the cytotoxic payload once internalized by the target cell, a mechanism exemplified by Brentuximab vedotin (Adcetris), used in lymphomas.
The exploration of new cytotoxic agents is also at the forefront, with a focus on drugs that are highly potent yet deliverable in lower doses to reduce systemic toxicity. Research in multifunctional ADCs is pioneering, aiming to deliver multiple therapeutic agents or merge diagnostic and therapeutic functionalities, akin to the concept of theranostics. Reducing the immunogenicity of ADCs involves molecular engineering to mask the ADC from the immune system, thereby preventing antibody-mediated clearance.
In manufacturing, the push is towards process optimization. The heterogeneity in the drug-to-antibody ratio (DAR) poses significant challenges, as seen with Mylotarg, the first approved ADC, which was initially withdrawn due to toxicity issues. Personalized ADC therapies, such as those targeting specific mutations or expression profiles in cancers, are a growing area of research, propelled by advances in genomic profiling technologies.
How do ADCs improve targeted drug delivery?ADCs have revolutionized drug delivery in oncology by utilizing monoclonal antibodies that specifically bind to antigens overexpressed in tumor cells. This specificity ensures targeted delivery of the cytotoxic payload, sparing healthy cells. For instance, ADCs like Trastuzumab deruxtecan have shown remarkable efficacy in HER2-positive cancers by exploiting this mechanism.
Minimizing side effects is another crucial aspect. Traditional chemotherapies indiscriminately attack rapidly dividing cells, leading to extensive collateral damage. ADCs, by contrast, deliver cytotoxic agents directly to tumor cells, as seen in Blinatumomab's targeting of CD19 in B-cell malignancies. This targeted approach significantly reduces the severity and incidence of side effects.
The increased potency of ADCs' cytotoxic agents, often microtubule inhibitors or DNA-damaging agents, allows for effective cell killing at lower overall systemic concentrations. The controlled drug release mechanism, a hallmark of ADCs, ensures localized drug release, reducing systemic exposure and toxicity. ADCs like Polatuzumab vedotin exemplify this, offering a more favorable safety profile compared to traditional chemotherapy.
Overcoming drug resistance, a significant hurdle in cancer therapy, is another area where ADCs show promise. By delivering cytotoxic drugs directly to the cancer cells, ADCs can bypass some mechanisms of drug resistance, such as efflux pumps commonly implicated in chemoresistance.
What are the challenges in developing ADCs?
The journey of developing ADCs is fraught with scientific and technical challenges. Target selection is critical; the target antigen must be highly expressed on tumor cells and minimally on normal tissues. Linker stability is a delicate balance, ensuring drug release at the tumor site while maintaining stability in circulation.
Drug potency and selection are crucial in ensuring efficacy at the delivered dose, necessitating a deep understanding of pharmacodynamics and pharmacokinetics. Homogeneity in ADC production is challenging, as variations in DAR can significantly affect safety and efficacy, highlighted by the initial challenges with Gemtuzumab ozogamicin (Mylotarg).
The therapeutic window of ADCs is narrow; achieving efficacy without unacceptable toxicity is a complex interplay of drug, antibody, and linker properties. Immunogenicity poses risks of reduced efficacy and adverse immune responses, necessitating sophisticated molecular engineering.
Resistance development to ADCs, through antigen modulation or other cellular mechanisms, remains a concern, necessitating ongoing research and development. Regulatory hurdles are substantial due to the complexity and novelty of ADCs, requiring comprehensive preclinical and clinical data to demonstrate safety and efficacy.
Cost implications are non-trivial; the intricate process of ADC development and production often results in high treatment costs, impacting accessibility and healthcare economics. Patient selection based on biomarker expression or genetic profiling is crucial for maximizing therapeutic efficacy, necessitating advanced diagnostic capabilities.
Conclusion
While the path of ADC development is laden with complex scientific, manufacturing, and regulatory challenges, the potential they hold in transforming cancer therapy is immense. As research continues to unravel the intricacies of these novel therapeutics, ADCs are poised to play a pivotal role in ushering in a new era of precision oncology, offering targeted, effective, and safer treatment options for cancer patients worldwide.
Get your weekly dose of industry news and announcements here, or head over to our Formulation portal to catch up with the latest advances in manufacture and therapeutic delivery.