Experts Investigate the Process and Formulation of Dry Powder Inhaled Drugs

We were very pleased to invite a wide range of formulation specialists to take part in our October discussion group. This month, the session’s topic focussed on the formulation of dry powder inhaler products. There has been a surge in interest in the pulmonary delivery and deposition of drugs for a variety of indications from allergic diseases to COVID-19, so it was great to see experts in this field come together to discuss this technology.
Formulation for Dry Powder Inhalation of Desloratadine
Yamini Shah, Associate Professor at L M College of Pharmacy, Ahmedabad, kicked off the discussion group by providing a brief introduction to her work on dry powder inhalers. The project that Shah embarked on started before the pandemic in 2020. She explained that after two or three months into the project, COVID-19 hit globally which presented a difficult obstacle at the time. Nevertheless, post-pandemic, Shah was able to show off the results from her research at our October discussion group.
The disease that Shah’s research focussed on was allergic rhinitis, an allergic response causing watery rhinorrhoea, airway obstruction, itching, sneezing and inflammation in upper respiratory tract. Shah noted that in severe cases of this condition, the inflammation may occur in lower respiratory tract. The work that Shah had produced aimed to explore a new dosage form which at the time was not available in India: dry powder inhalation.
Shah worked on the inhaled delivery of desloratadine as a dry powder formulation. The compound is a low molecular weight, low dose, tricyclic H1 antagonist. She explained that the rationale for using dry powder inhalers (DPIs) for desloratadine was that they can deliver the drug directly to the sight of action. Furthermore, the DPI makes no use of propellants or vehicles which makes it “environmentally safe.”
Shah then took us through a definition of dry powder inhalers: “they are devices which deliver a dry powdered formulation of an API for local and systemic action via a pulmonary route of delivery.” She explained that for local effect, the particle size should not be more than 5µm. Furthermore, for systemic effect particle size should not be more than 2µm.
Shah further stressed that devices should be developed taking into consideration children and patients with decreased lung function (as DPI efficacy depends on a patient’s inspiratory flow rate). This is an example of patient centricity, taking a patient’s needs into account in the design process of a drug device or formulation.
- Optimising Patient Centric Design for Inhaled Products
- Patient First: The Necessity of Patient-Centric Product Design for Enhanced Pulmonary Drug Delivery
Dry Powder Formulation
| Advantages | Disadvantages |
| • Physical and chemical stability due to powdered formulation. • Simple and patient friendly. • Easy to use. • Deep lung penetration in dry powdered form. • Available as unit dose, multiple dose, and multiple unit dose. • Free from propellants. | • Expensive. • Dose uniformity. • Dependent on patient's inspiratory flow rate. |
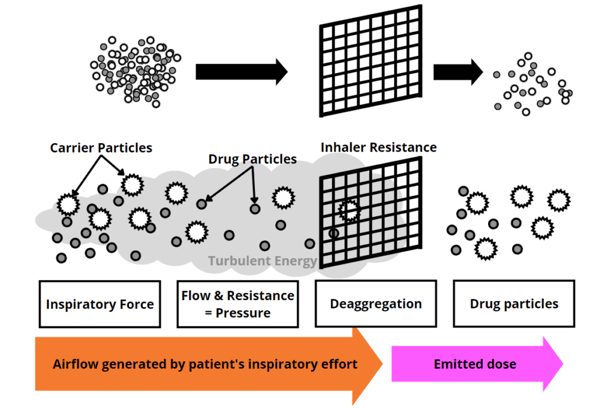
Shah explained that DPIs work through the turbulent energy created by the patient’s inspiratory effort. This inspiratory force pushes the drug formulation out of the device’s chamber in the form of aerosol mist. Furthermore, the resistance of the inhaler promotes deaggregation of the drug particles.
Shah then went on to outline the methodology and results of her research. She selected mannitol for the drug carrier due to its sugar alcohol which acts as an osmotic agent. Shah further explained that aerodynamic performance was also a contributing factor in the selection of the excipients.
Three methods were compared for the preparation of the DPI: colloid milling, spherical agglomeration, and physical mixture. Shah based her selection of the technique on particle size, flow properties, percent yield, percent water content, and aerodynamic performance. She concluded that spherical agglomeration would be the best suited for her need based on this comparison and then optimised the same using 32 factorial design.
Batches were formulated applying DOE, taking into account the critical factors: namely particle size, roundness, and aerodynamic performance of the formulation. The independent variables were then selected based on the process of making spherical agglomerates. All the factors were evaluated in three levels, low, medium and high. She showed that the data passed both dissimilarity and similarity range as per statistical analysis.
After the experimental and evaluation stages were complete, Shah was pleased to report a sound methodology and outcome: “It can be concluded from the present research that DPI of desloratadine can be successfully formulated,” Shah said. She further explained that “it gives efficacious aerodynamic performance and drug reach up to the alveoli region of the lungs.”
Creating Monodisperse Particles with Dry Powder Inhalers
Cees van Rijn, Professor of Nanotechnology and Microfluidics at the University of Amsterdam, was next to present to the attendees of the discussion group. Van Rijn explained why, in his view, it was important to investigate monodisperse powders. He said that due to the increasing interest in biologic formulations, it was necessary to ensure that their delivery was able to have a high lung deposition — “You need a lot of the drug in the correct place in the respiratory system,” van Rijn added.
To illustrate, van Rijn listed the typical inhaled delivery systems available to patients, along with the dose that they can be expected to deliver in milligrams (Figure 3). Van Rijn highlighted the fact that conventional nebulisers, dry powder – engineered particle, and soft mist inhalers were all able to achieve a dose of above 10mg. Van Rijn said that this was “reasonably important, because current formulations of medicines on the market can have doses of up to 30mg.”
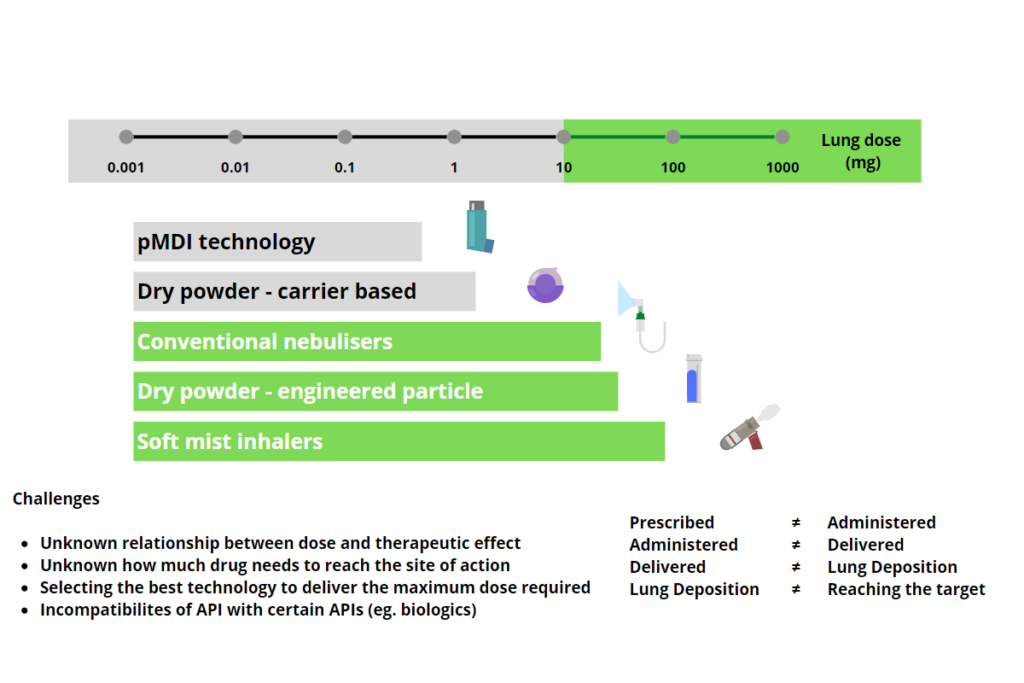
The main concern for van Rijn and his colleagues at the University of Amsterdam is to reach the correct site of action: “for some applications, you want the drug to go into the bronchi; for others, you want it to go to the alveoli.” He added that for each site of action, there will be a different recommended particle diameter. This is the reason why van Rijn and his team are focussed on creating monodisperse powders: improving the consistency of particle size will thereby improve the drug dose delivered to the correct site of action.
The current challenge of ultrasonic nebulisers, according to van Rijn, is that they produce a broad range of particle sizes — “how can we improve upon that?” he asked. Typical nebuliser nozzles create a conical distribution which breaks up into polydisperse droplets (figure 5 – left hand side). Van Rijn’s team used different nozzles with stimulated breakup, imposing an ultrasonic wave while the droplets emit. This technique was able to produce monodisperse droplets which then dry into monodisperse powder particles (figure 5 – right hand side).

Typical drop formation for a spray nozzle. 
Spray of 8 x 8 µm ? 16 µm spray droplets. 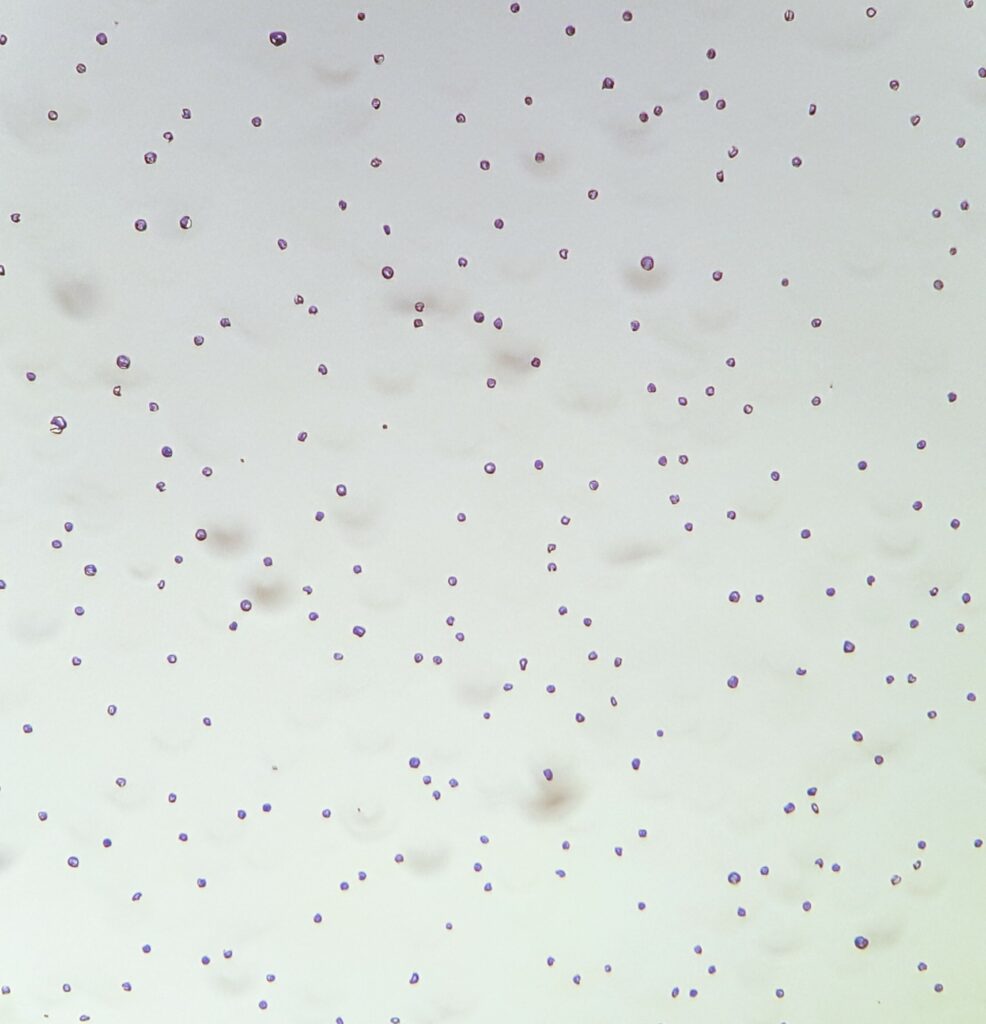
Monodisperse mannitol particles of 3-5 µm in size. Obtained with the 16 µm monodisperse droplet stimulated breakup nozzle device.
Van Rijn concluded by confirming that “it is really important to look for new methods to make monodisperse droplets; to get monodisperse powders, so that you can have better efficacy at the site of action.” The presentation section of our discussion group then ended and was followed by a stimulating conversation between our expert attendees. To see the full recording, be a part of our upcoming Formulation discussions, and have access to exclusive content, please consider our membership offerings.
Learn from and meet leading experts in pharmaceutical science, addressing the critical strategic advances and technical innovation in formulation, drug delivery and drug product development. Join us at Formulation and Delivery UK.