Potency Assays for Thalassemia and Sickle Cell Disease Gene Therapy Drug Products
Presented by: Riccardo Biavasco, Senior Scientist at bluebird bio
Edited by: Ben Norris
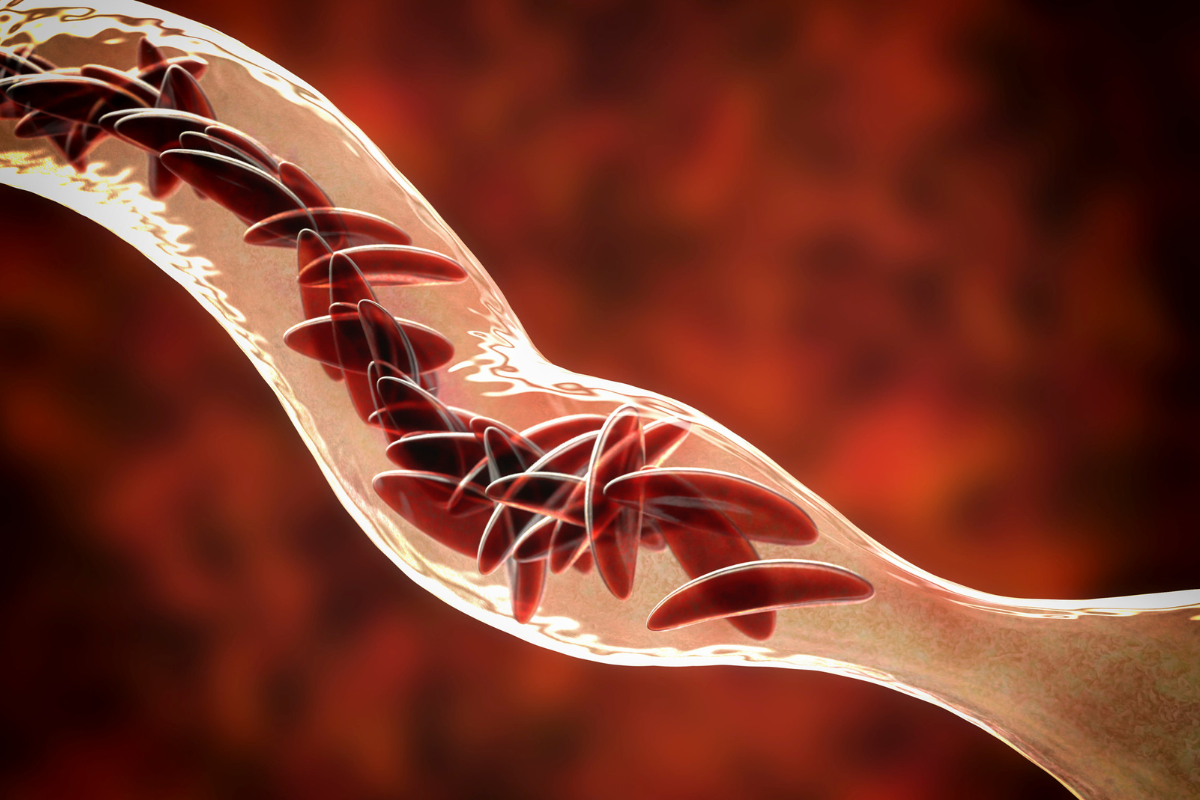
Diseases such as sickle cell anaemia – caused by a mutation that induces haemoglobin precipitation and subsequent sickling of red blood cells – can be treated through stem cell gene therapy. However, reproducing and quantifying the treatment process in vitro can be tricky, time-consuming, and expensive. Potency assays provide a means of testing and quantifying the efficacy of stem cell treatments. Riccardo Biavasco, Senior Scientist at bluebird bio, explains that assays that investigate the editing efficiencies are an effective and practical approach for testing and development of stem cell gene therapies.
Potency Assay Development for Cell Therapy
When it comes to the development of new treatments for cellular diseases like sickle cell disease, patient safety and treatment efficacy is paramount. “It's really important that we provide safe and effective therapies,” said Biavasco at Oxford Global's Cell Therapy Analytics Symposium in March 2022. Treatment efficacy is assessed through the use of potency assays, which are run to monitor the development of cell therapies and the suitability of drug products. “In our case these therapies are based on hematopoietic stem and progenitor cells (HSPCs), which are harvested thanks to mobilisation and apheresis,” he continued. HSPCs are modified to generate corrected red blood cells upon infusion, which ultimately provide the clinical benefits to ?-thalassemia and sickle cell disease patients.
“Once enriched with the CD34 marker, the cells are transduced with lentiviral vectors that integrate the therapeutic transgene,” Biavasco explained. Modified HSPCs are subsequently cryopreserved, then tested for safety and efficacy, after which they can be infused into their source patients. bluebird bio runs a suite of potency assays to demonstrate that the integrated transgene is able to stably express the therapeutic protein and correct the disease phenotype. One of the key determinants is the vector copy number (VCN), which ensures that an appropriate amount of the lentiviral vector (LVV) is integrated in the drug product.
In Vitro Cell Therapy Analysis
Biavasco then gave an overview of the physiologic process that bluebird bio's assays are modelling. “It all starts with the stem cells, the same ones that we want to correct in our patients,” he said. “These cells go through different steps of maturation, and they become more and more committed to the erythroid lineage until they start to really express the haemoglobin.” On reaching a haemoglobin threshold, the nucleus starts to condense, and once fully condensed is ejected from the cells.
- Discussion Group Report: New Developments in Upstream Bioprocessing
- Digital Twins: Innovative Modelling Techniques for Secure Research
- What's Next for Upstream Processing?
“It's one of the last steps in the maturation of red blood cells” said Biavasco. “So, this is what happens in vivo. We need to reproduce this in vitro, which is quite a challenge.” Fortunately, bluebird bio is up to the task and has developed a cell culture system that enables erythroid differentiation in vitro. In ?-thalassemia, cell growth and maturation are constrained by the absence of ?-globin. “Erythroid cells mature until they reach the point they really need haemoglobin, and there they get stuck,” Biavasco continued. The solution involves the administration of autologous CD34 hematopoietic stem cells to provide a continuous and durable source of corrected red blood cells.

These HSPCs are transduced with an LVV-encoding human ?-globin with an amino acid substitution (T87Q). This substitution confers anti-sickling properties to the haemoglobin derived from gene therapy – HbAT87Q – which can subsequently be quantified in the erythroid progeny of transduced HSPCs. Biavasco added that two distinct potency assays, tailored to each disease, are required to measure the impact of HBAT87Q expression. “What we want to see in our drug products is that once we add our therapeutic HBAT87Q, we can restore the physiologic maturation of red blood cells in vitro.” In ?-thalassemia, HbAT87Q corrects the maturation arrest, while also correcting for sickle cell morphology in sickle cell disease.
Potency Assays: Vector Copy Number is Top
Product potency is a key aspect of the overall process, as it provides a good indication as to whether the treatment is effective. Here, potency can be measured as a relative increase in the percent of mature erythroid cells or a relative decrease in the percent of sickled cells. Biavasco cautioned that it was not possible to show potency without accounting for the subject-specific background. “The absolute amount of in vitro mature erythroid cells or sickle cells deriving from the transduced cell is meaningless,” he said. “But as long as maturation percent increase or sickling percent decrease passes a specific threshold, the product is considered potent.”
Mechanism of action (MOA)-specific potency assays test for potential risks where a drug product contains LVV integrations that do not express the desired therapeutic protein or are are sequestered in a disproportionately small subset of cells. Testing for these risks necessarily increases the assay complexity, so there is a trade-off in information gained, time, and efficiency. “These assays can be measured in a semi-quantitative way,” said Biavasco. “But they come with a cost, and the cost is assay complexity.”
Part of the issue is the high impact of patient-to-patient variability, particularly with regard to the starting material. However, VCN is a valuable indicator to test for because it is simple, can be applied to many different diseases, and has a very quantifiable readout. “Cell editing measures are much stronger predictors of clinical efficacy compared to the MOA-specific readouts,” said Biavasco.
Future Indications and Applications for Potency Assays
One of Biavasco's main conclusions from the presentation was that the VCN is a strong indicator of treatment efficacy to monitor for in potency assays. “Vector copy number and percent transduced cells nicely trend together,” he said, “and one can predict the other.” Drug products with VCNs above specification reliably achieve high and stable HBAT87Q expression. VCN is predictive of clinical efficacy, which Biavasco described as a “challenging accomplishment” for cell and gene therapy drug products.
“Looking to the future, we would like gene therapy to be as accessible as possible."
“The VCN, and transduction measures in general, is our best predictor of clinical efficacy,” Biavasco said. Despite expressing the same therapeutic protein, ?-thalassemia and sickle cell disease require different MOA-specific potency assays. “In the end, the VCN correlates with more or less all the different potency assays,” added Biavasco. He rounded off by concluding that thoughtful reductions in testing complexity and cost can improve access to hematopoietic stem cell therapies for patients worldwide, while maintaining appropriate monitoring of drug products safety and quality. “Looking to the future, we would like gene therapy to be as accessible as possible to all patients in the world.”
Visit our Cell portal to read more articles investigating the applications of stem cell therapies and potency assays. If you'd like to register your interest in our upcoming Cell UK: In-Person event, click here.







