New MND Early Diagnostic Test: a 'Game-Changer' for Research on the Disease
Researchers at the University of Aberdeen in collaboration with the University of Edinburgh have developed a new test that could be a 'game changer' for the early detection of motor neurone disease (MND).
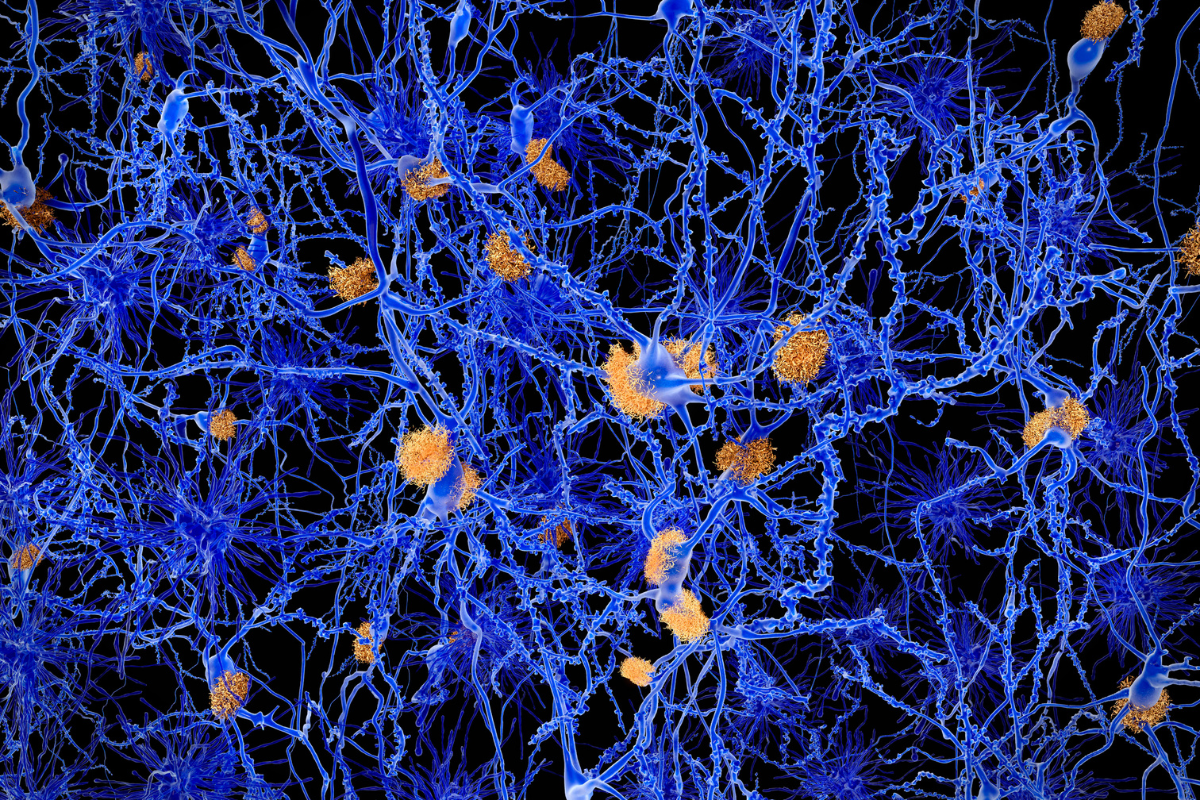
The test makes use of an RNA aptamer to detect the aggregation of a protein called TDP-43 in brain tissue samples. This aggregation can be detected before it interferes with the functioning of cells, and therefore before any symptoms present.
Aptamers have recently made breakthroughs in the diagnosis of cancer, but this is the first time that they have been used for MND. The disease currently has no cure, but earlier detection of MND can improve the care and management options that patients receive.
Furthermore, early detection allows for clinical trials of new medicines for MND to be conducted with patients at an earlier stage of their disease. Earlier stage clinical trials may help address the lack of effective medicines available for MND.
RELATED:
- Early Diagnostic Blood Biomarker for Dementia Identified Using Proteomics
- Investigating Biases in Diagnostics and Biomarkers: Three Case Studies
- Machine Learning Metabolomics Approach Used to Diagnose Ovarian Cancer
“Our findings have implications for early diagnostics and intervention prior to symptom onset in MND. With better ability to detect disease we might be able to diagnose people with MND earlier, when therapeutic drugs might be much more effective,” said Dr. Holly Spence, a Research Fellow at the University of Aberdeen.
The study, published in Acta Neuropathologica describes how TDP-43 is known to aggregate in patients with MND. However, postmortem analysis does not show aggregation correlating as predicted with the appearance of symptoms using traditional antibody tests.
TDP-43, when functioning normally, would repress the inclusion of a cryptic exon in the gene STMN-2. However, if TDP-43 is no longer functioning, this repression does not happen. Therefore, detecting incorrect splicing in the STMN-2 gene is a good marker for the loss of function of TDP-43.
But the intricacies of the link between the onset of the disease phenotype and advancement TDP-43 loss is not well understood. So the team used an RNA aptamer, TDP-43APT to identify the aggregation, and single molecule in situ hybridization to detect incorrect gene splicing associated with it.
The team found that TDP-43APT was able to identify instances of TDP-43 pathology and aggregation that would have been missed using traditional antibody stains. Identifying the presence of TDP-43 aggregation and STMN-2 cryptic exons could therefore form the basis of an early diagnostic test for MND, before any symptoms have been noticed.
Dr. Jenna Gregory, a Senior Clinical Lecturer at the University of Aberdeen, led the research group and commented on the implications of the study for MND diagnostics: "This tool ‘targets’ the disease protein and allows us to see where toxic clumps are building up in the body. It can do this for much lower amounts of disease proteins, and with greater accuracy than ever before."
She continued: “This could be a game-changer for MND research, diagnostics and treatment.”







