Identifying Prognostic Biomarkers for Follicular Lymphoma
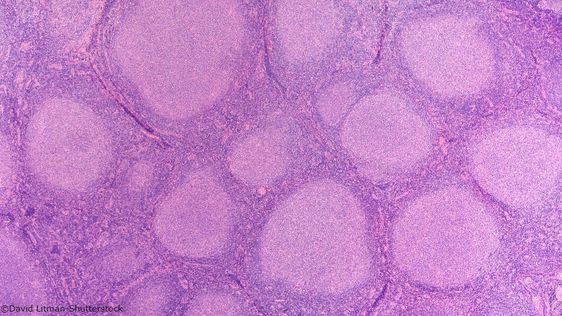
Follicular lymphoma is a cancer of the B-cells and represents approximately 30% of non-Hodgkin lymphomas. The disease affects up to 2150 people in the UK each year and follows an indolent but unpredictable course. Whilst the majority of patients experience long-term survival, approximately 20% undergo early treatment failure and relapse within 24 months of starting therapy.
The group of patients who relapse within the first two years have a 35% increased risk of death within a 5-year period. To help reduce this statistic, it is imperative to be able to identify those who will potentially fall within this patient population as early as possible to enable the introduction of optimised therapy regimens. Prognostic biomarkers of early relapse can then be translated into markers for overall survival. At the University of Manchester, Martin Fergie, Lecturer in Healthcare Sciences, and his team are trying to do just that.
Fergie and his team are committed to identifying such biomarkers to facilitate escalated treatment regimes. Understanding the diversity of spatial interactions within the tumour immune microenvironment paves the way for unlocking the next generation of prognostic biomarkers for follicular lymphoma. Using, multiplex immunofluorescence imaging facilities that measure multiple antigen markers at the single-cell level whilst maintaining the spatial context of the cells intact, the team hope to discover a novel biomarker using a novel methodology named hypothesised interaction distribution.
Digital Pathology and Artificial Intelligence
“Pathologists in clinical practice are the gold standard in cancer diagnosis,” Fergie explained. Typically, pathologists will collect and analyse tissue samples taken from a patient to decide on a diagnosis. Increasingly, analysis requires more complex protocols, which call for artificial intelligence (AI).
The opportunity of digital pathology lies in its ability to perform analytical and diagnostic tasks on par with human experts in terms of accuracy.
“Immunohistochemistry assay analysis is becoming more and more quantitative,” Fergie added. “The types of questions and analysis pathologists are being asked to perform has induced digital adoption into the clinic.” For instance, it is now possible to produce digital images which can be used instead of an optical microscope. This means pathologists can perform their diagnostic work using a digital workstation.
Innovations have paved the way for the adoption of image analysis and AI algorithms over purely or semi-quantitative assessment methods for detecting cell nucelli and different regions of the tissue within the sample. The potential of digital pathology lies in its ability to perform analytical and diagnostic tasks on par with human experts in terms of accuracy. Some of the most promising areas of digital pathology applications include cell phenotyping, tissue segmentation, and rare object detection.
Digital Pathology and Spatial Context
Digital pathology also provides a new opportunity for disease biomarkers. In particular, digital pathology can be harnessed as an analytical tool to examine spatial contexts such as proteomics and measure antigen expression on cells to conduct cell phenotyping. “Cells can be detected and phenotyped within the context of the wider tissue,” Fergie explained.
Whilst some of this analysis is commonly performed using flow cytometry, there are limitations. “Two things tend to happen: you cannot also be sure of the quality of the sample retrieved, and you lose spatial context,” he continued. For instance, whilst tests such as flow cytometry can accurately count cell types, tissue structure and distribution understanding are lost. To counter this issue, Fergie and his lab propose using multiplex immunofluorescence imaging to keep the cell context intact.
- Building Digital Twins of Disease Pathways
- The Latest Applications in Digital and Wearable Biomarkers
- Overcoming the Regulatory Challenges of Digital Health Technologies
Their methodology is as follows: follicular lymphoma tissue samples from the tumour microenvironment are stained with cells being detected and phenotyped based on antibody expression profiles using applied image analysis algorithms. Finally, interactions between phenotypes are then modelled based on their proximity in the tissue.
The platform used allows for six antibody markers plus a DAPI marker which functions as a fluorescent stain binding strongly to adenine-thymine-rich regions of DNA. Speaking further on the methodology, Fergie clarified that “signs of interaction meant we could start to study whether or not the difference in activities have an impact on a patient’s outcome.”
Prognostic Risk Biomarkers for Follicular Lymphoma
Fergie and his team applied this multiplex immunofluorescence method on a cohort of 127 follicular lymphoma patients at The Christie Hospital Trust to identify potential biomarkers for overall and progression-free survival as well as relapse within 24 months. Results also assessed additional prognostic value compared to Follicular Lymphoma International Prognostic Index.
Diagnostics biopsies were stained using multiplex immunofluorescence protocol, and the diversity of the tumour microenvironment quantified using entropy calculation. “We used an interaction matrix as a candidate biomarker and demonstrated that a diverse immune infiltrate leads to better survival outcomes than an immune infiltrate with low diversity,” Fergie said. Differences were also observed in the tumour microenvironment between the progression of disease in 24 months (POD24) group and the negative POD24 groups.
Future Outlook
“The diversity of interactions found meant we were about to predict both overall survival and progression-free survival,” he explained. “We concluded that there is a potential to predict disease outcomes in this setting”. Looking ahead, Fergie and his team are committed to furthering their research into Follicular Lymphoma markers and continuing their fight against the prevalence of non-Hodgkin lymphomas.
They aim to evaluate biomarker efficacy on an independent cohort exclusively treated to modern standard and hope to perform assay validation to demonstrate repeatability. Identifying additional applications in other disease areas will also shape the future of their investigations.
Want to stay up to date with the latest Biomarker news? Register now for Oxford Global’s flagship event, Biomarkers US: In-Person. This is a must-attend forum covering the latest trends transforming biomarker and translational research







