Biomarker Strategies for Monitoring the Tumour Microenvironment
The use of biomarker strategies for monitoring the tumour microenvironment is integral to assessing the proper function and performance of new and upcoming treatments for diseases such as lymphoma. Here, we look at how a multitude of approaches can be developed and applied to studies of the tumour microenvironment for the investigation and development of a suitable biomarker strategy. Two presentations from Oxford Global’s flagship Biomarkers 2023 event highlighted the extent to which new approaches are being pioneered for a host of different applications with a focus on the tumour microenvironment.
Multiplex Immunofluorescence for Quantifying the Tumour Microenvironment
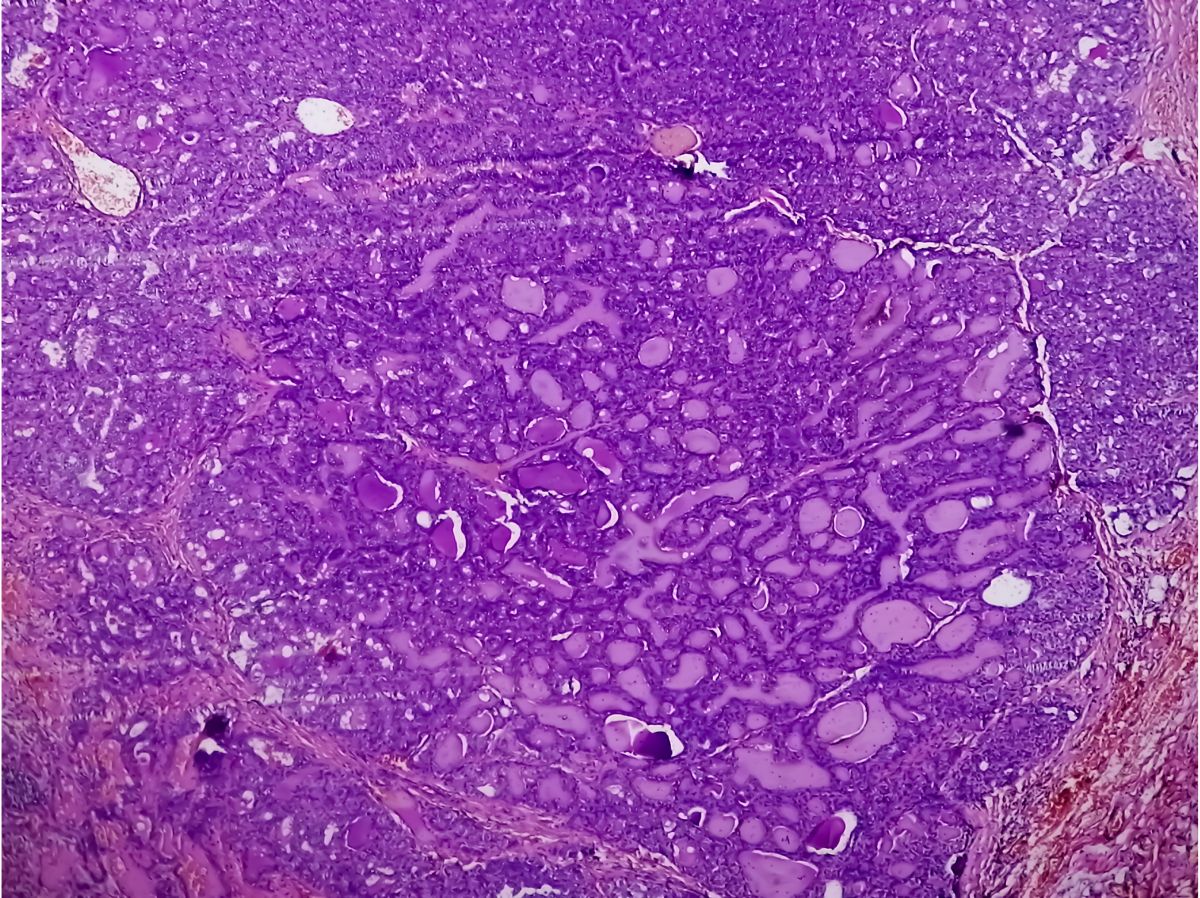
Follicular lymphoma – a variant of non-Hodgkin lymphoma – develops when the body makes abnormal B lymphocytes. When a patient develops a lymphoma, the abnormal lymphocytes build up in the lymph nodes or in other body organs. Martin Fergie, CEO of Spotlight Pathology and Lecturer in Data Science at the University of Manchester, has been investigating the behaviour of the tumour immune microenvironment in lymphoma. Along with colleagues at The University of Manchester and The Christie NHS Foundation Trust, he has developed an image analysis biomarker method based on multiplex immunofluorescence to study how spatial interactions within immune cells in the tumour microenvironment can have an impact on patient outcomes.
Fergie explained that follicular lymphoma represents around 30% of non-Hodgkin lymphomas, affecting around 2,000 people in the UK each year. “It follows an indolent but unpredictable course,” he said of the disease. “Most patients can live with it for a long time through well-managed therapy, but 25% of patients who undergo early relapse have much worse survival outcomes in the long term.” As a result, there exists a pressing need to identify the group of patients predisposed to worse outcomes, with consideration given to escalated therapy regimes in that area.
The current marker used for risk stratification in follicular lymphoma is FLIPI (the Follicular Lymphoma International Prognostic Index). “It’s a very well-proven biomarker, but it’s not a sufficiently powerful tool to be used for early therapy decisions,” said Fergie. As a result, his team has been working towards the identification of a risk stratification biomarker to try and identify a predisposition towards early relapse within the broader follicular lymphoma patient population. “We also wanted to give additional value to FLIPI for follicular lymphoma,” Fergie added. The endpoints he used for this were overall survival, progression-free survival, and whether the patients relapsed in 24 months.
Multiplex Panels and Immunology in Follicular Lymphoma
Fergie’s study focused on a population of follicular lymphoma patients receiving treatment at the Christie Hospital in Manchester. His approach involved a multiplex immunofluorescence panel, which was stained and used to stratify the fluorescent markers within tissue samples. The central aim of this method was to identify the diversity of interactions within the tumour microenvironment and quantify them accordingly.
Fergie explained that the idea for this work and approach came from some earlier, more qualitative work which looked at spatial patterns in immune cells via microscopy. “Survival patterns were identified through that approach,” said Fergie, “and we’re interested in developing a method to do that quantitatively.” The investigation went through a rigorous validation process, where each multiplex antibody was validated against a single-plex section to ensure good correlation in terms of expression levels across the whole cohort of antibodies. A key focus involved developing a cell segmentation approach for analysing lymphoma samples, which often have densely-packed nuclei compared to other tissue types.
Once the nuclei were identified, Fergie’s team grew a membrane area, before measuring intensity across the two compartments of the nucleus and cytoplasm area. Cells were detected and phenotyped, with individual thresholds applied to both the antigens and antibody markers under the supervision of a pathologist. Researchers manually identified cell populations by looking at known concentrations of antibodies. “The reason we didn’t opt for a more data-driven approach is we ended up with a combinatorial problem that’s hard to validate, along with a lot of candidate cell types,” Fergie explained.
Quantifying Interactions via Immunofluorescence Biomarkers
The core principle behind analysis of cell interactions involves looking at the distance between using cells from two different phenotypes, or even from the same phenotype. Once the location has been derived, researchers could use an X/Y coordinate of its location in the tissue – typically measured in micrometres – and a vector of the stain intensity for each marker. “We’re interested in quantifying an interaction distance,” continued Fergie. “We put all this information into a hypothesised interaction matrix to see across the sample.”
Regarding the study’s results, the priority was to validate the same overall survival effect as witnessed when the first biomarker was investigated. The results showed that the diversity of the immune microenvironment had a protective effect on overall survival. Individual cell populations of macrophages and T-regulatory cells also showed promising results as candidates for potential biomarkers for follicular lymphoma in this context. For Fergie, the next step will involve moving towards including CDC macrophages as an endpoint in clinical trials. “We’ve obviously got a lot of assay validation work to do there so we can demonstrate getting it set up in a repeatable environment,” he concluded.
Interpreting Immune State to Drive Biomarker Strategies for Treatment
In the context of the tumour microenvironment, suitable biomarker strategies can also be driven by a hypothesis – if that hypothesis is well-founded and sensibly applied. In this context F-Star Therapeutics have been developing their flagship bivalent molecule FS222, a novel CD137/PD-L1 tetravalent bispecific antibody which modulates the preclinical tumour microenvironment by activating CD8+ T cells. The two targets for this molecule are CD137 and PD-L1.
- Interview: Genentech's Simon Gao discusses the impact of AI on biomarker discovery
- Could neuroimmune proteins hold the key to neurodegenerative disease diagnosis?
- Biomarker testing through multiplex immunofluorescence
F-Star’s technology focuses on antigen binding sites, using tetravalent bispecifics to activate the body’s immune system. CD137 promotes the activation and survival of T cells, while interactions with PD-1 result in T cell immune suppression. The functionality of FS222 aims to drive a clustering of CD137 on the target cell to increase its life and drive activation.
Functionality and Implementation of Biomarkers for Immune Therapy
Initial results from a preclinical trial suggest that labels observed were in-line with the modelling predicted for a particular antibody, with the project’s research focus now moving to soluble biomarkers. No apparent plateau was reached in soluble receptor levels at the dose levels analysed. A surrogate mouse antibody with a mechanism matched to FS222 witnessed significantly reduced tumour growth with greater survival benefits than a combination of monospecific mAbs. Changes in key biomarkers were seen in both mouse and cynomolgus macaque studies, which aided in the creation of translational hypotheses.
The next steps for the development of FS222 will utilise a robust biomarker strategy to support selection of an optional dose and schedule for efficacy cohorts. Biomarker strategies introduced in this way help to interpret the drug’s mechanism of action regarding both the target and all markers involved. Among the considerations to build into a clinical trial, one of the most important is pharmacodynamic markers, as these allow for the assessment of whether the compound reaches the target in treated patients. By incorporating relevant biomarker strategies into discovery and development at the earliest stages, developers of new therapeutics can help to track and ensure efficacy in drug candidates.
Want to read more about the applications of multi-omics techniques in biomarker discovery and analysis? Head over to our Biomarkers newsfeed for regular updates on the latest trends in the field. If you’d like to learn more about our upcoming Biomarkers UK conference, visit our event website to download an agenda and register your interest.







