Japanese Team Successfully Skip Abnormal Gene In Vitro With Antisense Oligonucleotide for BPAN
A genetic disorder called beta-propeller protein-associated neurodegeneration (BPAN) causes progressive neurodevelopmental issues and is characterized by a build-up of iron in the brain (substantia nigra and in the globus pallidus).
It is a very rare disease, effecting approximately 500 people worldwide and is caused by genetic mutation on the WDR45 gene on chromosome Xp11. There are currently no therapies for BPAN, although there are medications that can help manage the symptoms of the disease.
RELATED:
- Innovation at the Crossroads: Oligonucleotide Therapeutics and the Evolution of Drug Design
- How Do Regulatory Considerations Impact the Clinical Development of Oligonucleotide Therapies?
- New Approach to Oligo-Peptide Synthesis from Novo and Aarhus University
BPAN can be caused by a variety of pathogenic variants of the WDR45 gene. Researchers from three Japanese universities: Keio University School of Medicine, Tokyo, Kobe Gakuin University, Kobe, and Kyoto University, Kyoto, have used an antisense oligonucleotide (ASO) to skip the faulty gene in an in vitro model.
The specific genetic variation in question is that of a 17 year old Japanese female patient who expressed impaired motor function, and developmental delay since birth. At 15, MRI revealed iron deposits in her brain (substantia nigra and globus pallidus), consistent with a diagnosis of BPAN.
Whole genome sequencing and RNA sequencing identified the specific genetic variation that the patient had: WDR45 (OMIM #300526) chrX(GRCh37):g.48935143G > C, NM_007075.4 (NM_001029896.4/ENST00000376372.9):c.235 + 159C > G.
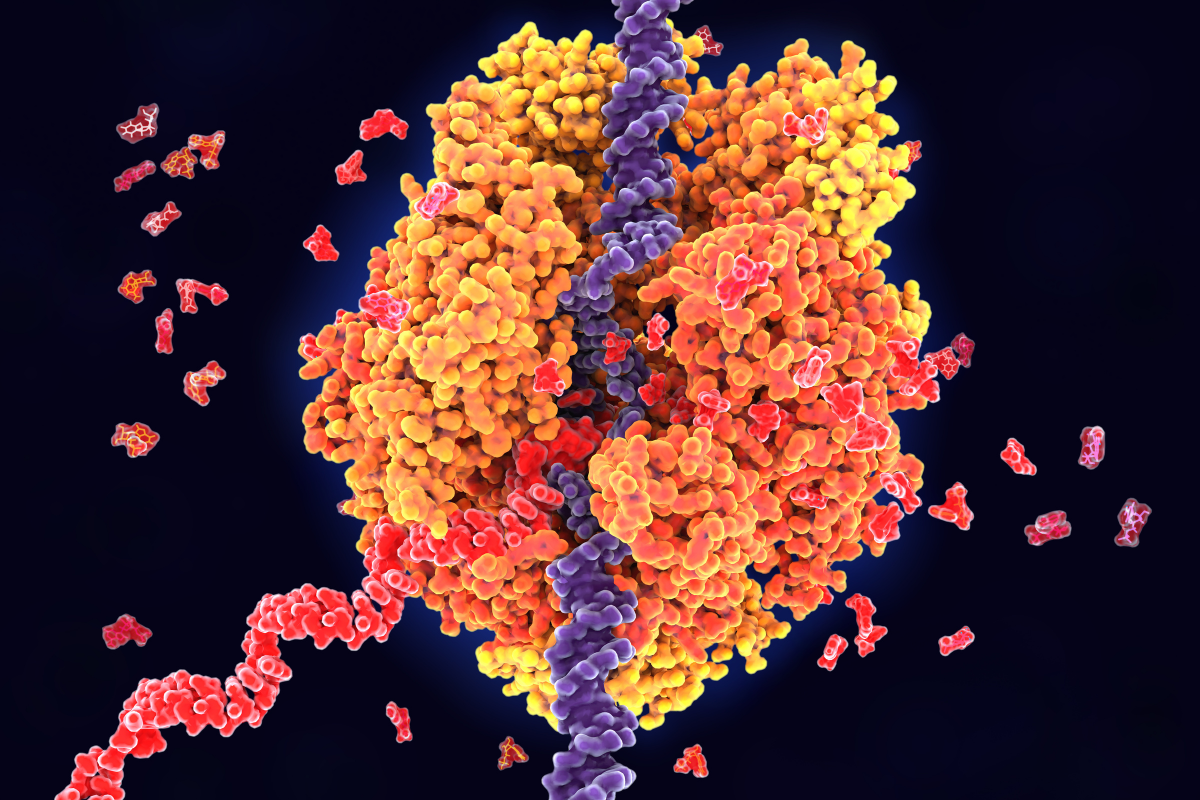
Further investigation showed that the cause of BPAN was a result of pseudoexon insertion remote from the exon–intron junction. The paper, published in Scientific Reports says:
"The fact that pseudoexon insertion is the cause of BPAN indicates that inducing pseudoexon skipping during splicing would normalize the patient's gene product, and that an antisense oligonucleotide (ASO) that induces pseudoexon skipping could be a treatment for this BPAN case."
The team then went looking for an antisense oligonucleotide that would cause the faulty part of the genetic sequence to be skipped, and thereby provide a therapeutic option for BPAN.
To do this, the group used a reporter system that they had recently developed using two different fluorescent proteins: "mCherry, a transfection marker designed to facilitate evaluation of exon skipping and split eGFP, a splicing reaction marker."
mCherry helped them see when cells take up the genetic material they're testing. And split eGFP, helped them track the process of splicing, where introns are removed, and exons are joined together in RNA.
The group's initial screening synthesised 15 ASOs and evaluated them based on their ability to skip pseudoexons, and thereby restore normal gene function.
After further screening, they identified a 24-base ASO, WDR45In5#6-5-24: caaccuucucaagcuauaagaucc, which had the best efficacy of skipping the abnormal pseudoexon. The sequence was then selected as a candidate for further development.
The team hopes that the data presented in their paper will provide the necessary evidence to continue investigating their candidate in preclinical in vivo studies. Looking further into the potential of ASO therapies for the treatment of rare diseases shines a light on the unmet needs that patients and clinicians are desperate to address.