Using Live Gut Bacteria as a Co-Therapy for Checkpoint Inhibitors
Edited by Tom Cohen
At Preclinical Oncology: Online, Ghaith Bakdash, Director of Cell Biology at Microbiotica gave a fascinating presentation which outlined the development of his company’s therapeutic. MB097 is a co-therapy for anti-PD1 checkpoint inhibitors and is set to enter phase Ib clinical trials.
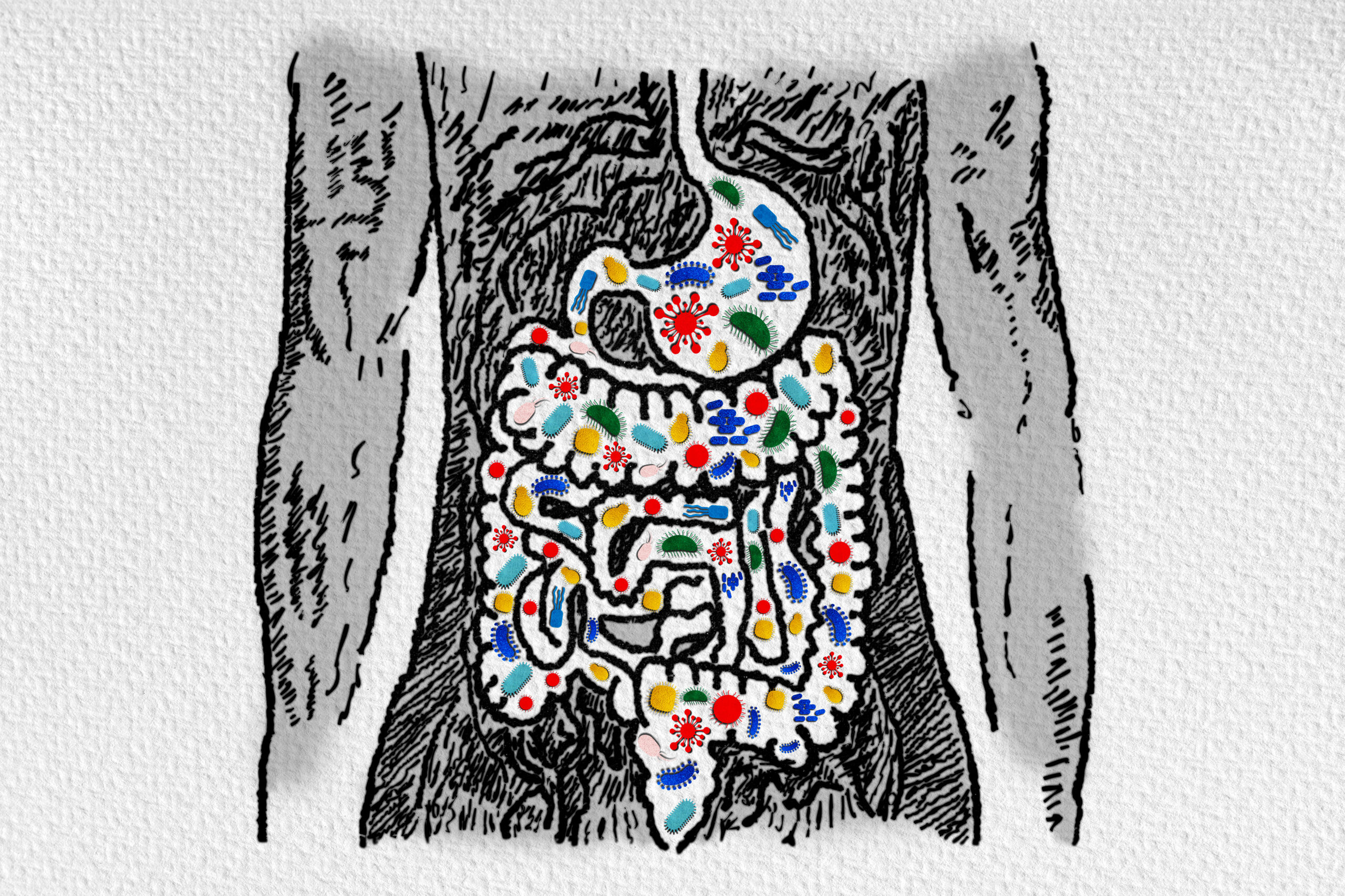
Microbiotica develops bacterial based therapeutics by linking changes in the human microbiome to clinical outcomes. Dr. Bakdash explained that the company uses its bacterial genomic database to define microbiome composition in relevant patient groups. Microbiotica’s in-house bioinformatics platform can then identify microbiome signatures linked to patient outcomes, allowing for the development of live bacterial therapies.
“All this made possible by our own unique microbiome discovery platform,” said Dr. Bakdash. Not only does the company define the microbiome make-up of patients, but it also isolates the patients’ bacteria which contributes to their personalised bacteria bank.
Microbiotica is in possession of an enormous proprietary collection of bacterial strains “all of these are potential therapeutics,” added Dr. Bakdash. The company has also constructed its own reference genome database which allows for “deep and precise determination of microbiomes.” Microbiotica’s database is ever-growing and based on global samples.
Melanoma IO Program: MB097
The therapeutic candidate developed by Microbiotica is intended to fill the gap in efficacy of immune-checkpoint-inhibitors (ICIs) when it comes to melanoma indications. ICIs have revolutionised treatments of multiple malignancies by increasing long term survival rates. For melanoma patients, this increase in the survival rate is high, but still only 40 to 50% benefit.
“There is a major need for a co-therapy to increase the response rate to ICIs,” described Dr. Bakdash. Mouse models have shown that faecal microbiota transplants (FMT) from responsive patients to a tumor-bearing mice can increase the efficacy of ICIs in those mice. Dr. Bakdash added that further evidence has corroborated this effect in humans, rendering non-responding patients responsive via FMT from responding patients.
The challenging factor, according to Dr. Bakdash, is that there has been no consensus on the bacterial species that cause this effect. “There have been five clinical studies that report different species that could be involved in boosting response to ICIs,” explained Dr. Bakdash. He added that combining the analysis of these five studies has also proven ineffective at narrowing down the effective species.
To resolve this conundrum, Microbiotica launched its own study named MELRESIST in collaboration with Cambridge University Hospitals. Dr. Bakdash specified that MELRESIST had the largest number of patients in comparison to the previous studies: 69. Stool samples were collected from melanoma patients before and throughout ICI therapy, those samples were all processed and analysed using Microbiotica’s in-house bioinformatics tool.
By combining the data from the MELRESIST study with three other published studies, Microbiotica managed to generate a common signature that can predict patient response to ICIs with 91% accuracy. This common signature can be developed into a biomarker and was used to develop a live bacterial therapeutic.
MB097: A Live Bacterial Therapeutic to Induce Tumour Killing by Activated CTLs
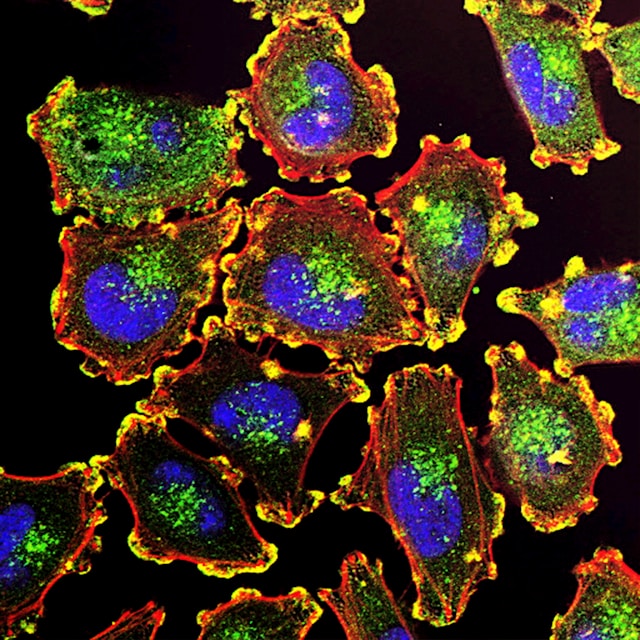
The results of the melanoma studies returned nine bacterial species identified as being associated with response to ICIs and consistently more abundant in responsive patient. These were developed into their therapeutic: MB097. Dr. Bakdash detailed Microbiotica’s attempts to validate the anti-tumour efficacy of MB097 by addressing dendritic cells/Cytotoxic T Lymphocytes (CTLs) axis.
Dr. Bakdash outlined the mechanism by which MB097 can support the effect of ICIs. MB097 can activate dendritic cells, in doing so, it skews the cytokine production from the immune inhibiting IL-10 toward the activating cytokine IL-12, “which has an important role in activating CTLs.”
Microbiotica then wanted to verify whether dendritic cells treated with MB097 could give rise to activated CTLs. The researchers assessed this by investigating the production of interferon-? and granzyme B by activated CTLs, which Dr. Bakdash reported as a success. Finally, the company verified whether the activated CTLs were functionally capable of killing tumour cells, which was also a success.
The final part of validating the therapeutic was to assess the capability of MB097 to have anti-tumour effects in vivo. Microbiotica used a MCA205 syngeneic model in SPF mice to do this. The mice were treated with antibiotics and then MB097. Dr. Bakdash reported that the results of the study showed the combination of MB097 and anti-PD1 ICI managed to slow tumour growth far more than control groups.
Running a New Observational Study Called MITRE
Microbiotica is now running a new observational study called MITRE, which is similar to MELRESIST but operates on a much larger scale. MITRE is being run in collaboration with Cancer Research UK, involving 12 centres in the UK. Enrolment started in July 2020, aiming at recruiting 1,800 patients undergoing ICI therapy and this time will be looking at non-small cell carcinoma and renal cell carcinoma in addition to melanoma.
Join us at Immuno UK: In Person and gain valuable insights into the approaches impacting the immunotherapy field through 40+ outstanding presentations tackling key discussion points in immuno-oncology, immunology, and inflammation.
Sign up for our Immuno newsletter to receive the highlights of our Immuno content, upcoming events, and more.