Are Neuroimmune Proteins the Key to Neurodegenerative Disease Diagnosis?

A new research study from Boston University’s Chronic Traumatic Encephalopathy Center suggests neuroimmune proteins may serve as a diagnostic biomarker for certain neurodegenerative diseases. Published in the Journal of Neuroinflammation, the research found that neuroimmune proteins can differentiate between tauopathies.
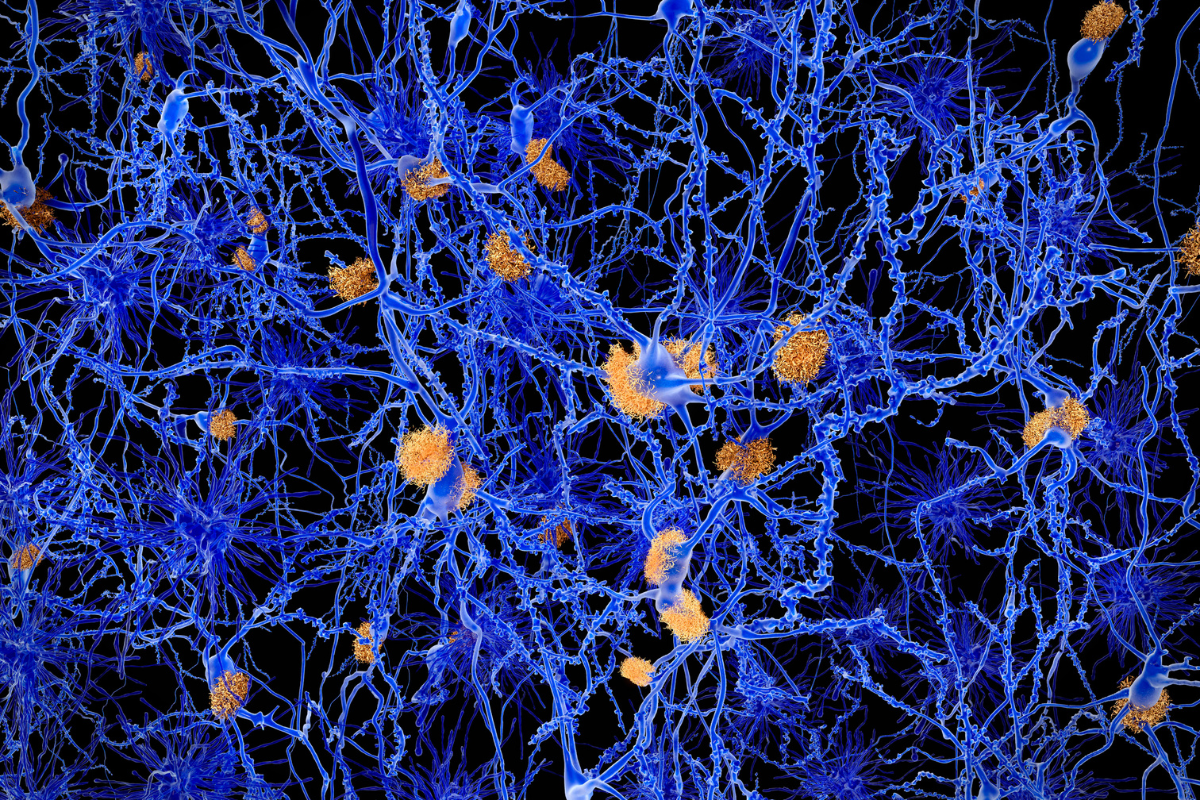
Tauopathies are a group of neurodegenerative diseases characterised by the pathologic accumulation of the hyperphosphorylated tau protein. Whilst the most recognised form of tauopathology is Alzheimer’s disease (AD), chronic traumatic encephalopathy (CTE), progressive supranuclear palsy (CTE), corticobasal degeneration (CBD), and argyrophilic grain disease (AGD) also all present significant health risks.
- Digital Biomarkers: Using Smartphones for the Passive Monitoring of Neurodegenerative Diseases
- Fluid Biomarkers for Neurodegenerative Disease
- Human Stem Cell Models of Neurodegeneration: Exploiting In Vitro Phenotypes to Support Drug Delivery
The study aimed to investigate the specific molecular factors driving each distinct tauopathy. This is in response to an evident lack of known biomarkers differentiating each disease. Prior research has likewise indicated that neuroinflammatory changes could offer a novel resource for potential biomarkers and mechanistic targets.
Boston University’s Chronic Traumatic Encephalopathy Center set out to address the challenge of identifying and treating tauopathies during a patient’s lifetime. Many diagnoses are restricted to after death. To examine each tauopathy, the study used “a 71 immune-related protein multiplex ELISA panel...to analyse anterior cingulate grey matter from 127 individuals neuropathologically diagnosed with AD, CTE, PSP, CBD, and AGD.”
Next, a partial least square regression examination was performed to ensure unbiased clustering and identify correlational proteins. This was followed by receiver characteristic and binary logistic regression analysis. Finally, “validation in postmortem cerebrospinal fluid (CSF) from 15 AD and 14 CTE cases was performed to determine if candidate proteins could act as possible novel biomarkers.”
Results showed that the protein CCL21 successfully distinguished CTE from AD in spinal fluid. This provided a compelling case for the protein’s potential as a novel biomarker for in-life diagnosis. Researchers concluded, however, that a single all-determining protein diagnostic biomarker is not likely to exist.
Results showed that the protein CCL21 successfully distinguished CTE from AD in spinal fluid.
Protein coupling, along with combination biomarkers such as imaging studies and clinical symptoms, will be necessary. Nevertheless, the significance of the study results is not lost. The corresponding author Jonathan Cherry, Research Health Scientist at the VA Boston Healthcare System and Assistant Professor of Pathology and Laboratory Medicine at Boston University Chobanian & Avedisian School of Medicine explained how the results “provided more targets that can help increase the overall specificity of diagnosis.”
According to Cherry, the research efforts highlighted the importance of the immune system to neurodegenerative disease. The hope is that a more conclusive understanding of the neuroinflammatory signature of each individual disease will help identify more specific biomarkers and will ultimately lead to the discovery of novel therapeutic compounds.
Jonathan D. Cherry et al, Neuroimmune proteins can differentiate between tauopathies, Journal of Neuroinflammation (2022). DOI:10.1186/s12974-022-02640-6
Want to stay up to date with the latest Biomarker news? Register now for Oxford Global’s flagship event, Biomarkers UK. This is a must-attend forum covering the latest trends transforming biomarker and translational research.
Get your weekly dose of industry news here and keep up to date with the latest ‘Industry Spotlight’ posts. For other Biomarkers content, please visit the Biomarkers Content Portal.