Novel Targets and Studies in Immunology and Autoimmunity: Antigen-Specific Immunotherapy and Therapeutic Chaperones
Immuno UK 2022 featured two great presentations about autoimmunity and immunology. David Wraith, Professor of Immunology and Director of the Institute of Immunology and Immunotherapy at the University of Birmingham, presented his talk on Antigen-Specific Immunotherapy of Autoimmune Diseases. Secondly, Paul Eggleton, Professor of Immunology at Exeter University, and Senior Director of Immunology at Revolo Biotherapeutics, expounded the immunomodulatory function of chaperones in the endoplasmic reticulum to make novel therapeutic agents.
Antigen-Specific Immunotherapy Of Autoimmune Diseases
Wraith’s presentation focused on antigen-specific immunotherapy for autoimmune disease, a technique that allows for the modification of disease without the reliance on non-specific immune suppression. “Anybody treating patients in autoimmunity will know the hazards of long term immune suppression,” explained Wraith. He added that the pandemic has shown how immunosuppressed patients have to retreat from society to shield from pathogens.
The pressing need to improve immunotherapies for autoimmune disease has led Wraith’s team to investigate antigen-specific approaches of which Wraith described various attempts.
Liposome carriers, red blood cell carriers, and nanoparticles have also been employed to induce tolerance — both with and without the help of immunosuppressing drugs. Wraith explained that this approach comes from the belief that injecting an intact antigen will cause an activation of immune response and exacerbate disease.
Expanding on this concept and taking it to the next level, Pere Santamaria has experimented with the administration of nanoparticles coated with major histocompatibility complex (MHC) and peptide. This induces effective Tr1-mediated immune regulation and has been highly effective in experimental animal models. The approach still remains to be tested in the clinic, however.
Introducing the use of peptide antigens, Wraith said: “I believe the most straightforward and simple approach is using the peptides themselves.” One method uses Imcyse modified peptides with high redox potential to promote cytotoxic activity in CD4+ T cells. The Apitope approach uses T cell epitopes designed to mimic naturally processed antigens and only modified to optimise solubility.
Critical Questions
Wraith explained that there are three critical questions to keep in mind for antigen-specific immunotherapy:
- What is the mechanism of action?
- Which approach induces bystander suppression?
- Which approach permits repeated antigen administration?
Bystander suppression
A core concept for Apitope’s approach is the phenomenon of bystander suppression which Wraith described as: “the induction of tolerance to antigen A within a tissue that spreads to suppress the immune response to antigens B, C, and D from the same tissue.”
This powerful concept proved particularly useful when Wraith’s team found that bystander suppression could be induced by synthetic peptides. Later, this was confirmed by Pere Santamaria’s work using MHC-peptide coated nanoparticles to suppress autoimmune liver disease in model systems.
What is an Apitope?
There are however criteria for which epitopes will provoke tolerance when administered in solution. These epitopes must be highly soluble in order to selectively reach steady-state dendritic cells. Furthermore, these peptides must be able to mimic naturally processed epitopes. Peptides that are able to bind to the MHC are defined as antigen processing independent epitopes or apitopes.
Mechanism of Action
Peptides that are designed to bind directly to MHC and are soluble enough, rapidly seek out and become presented by steady state dendritic cells. This induces anergy in naïve and effector T cells and promotes the differentiation of Tr 1 cells and effector Treg cells expressing FOXP3. Both of these cell subsets upregulate inhibitory receptors and switch their transcription factor expression, upregulating CMAF and NFIL3.
This promotes IL-10 production via an epigenetic mechanism which results in downregulation of the antigen presenting machinery of dendritic or other antigen presenting cells. The upshot of this is the suppression of immune response through bystander suppression.
Location, Location, Location Governs the Immunomodulatory Functions of Therapeutic Chaperones
The next presentation was given by Paul Eggleton, Hon. Professor Immunology at Exeter University and Senior Director of Immunology at Revolo Biotherapeutics. Revolo’s approach to immunotherapy exploits chaperones in the endoplasmic reticulum (ER) which aid in protein folding inside cells. ER chaperones are potent immune modulators outside of cells and can be used to treat cancer or autoimmune diseases.
Eggleton described two proteins that Pharma are exploiting in this way: calreticulin, which is often presented on the plasma membrane of tumour cells, and BiP (or GRP-78), which Revolo are testing in clinical trials is responsible for aiding immune tolerance in many autoimmune diseases. “This generation of proteins could be the next generation of ‘immune resetting’ therapeutics,” said Eggleton.
Intracellular Chaperone Function of Calreticulin and BiP
Calreticulin interacts with unfolded proteins when they are released from a ribosome in the ER. Eventually the correctly folded proteins get processed, glycosylated, and allowed to leave the cell if it is of sufficient quality or degraded if not. Similarly, BiP can interact with protein disulphide-isomerase to allow these proteins to disaggregate, aggregate, and effectively act as quality control chaperones to correctly fold proteins.
An important focal point of Eggleton’s presentation was the fact that the function of calreticulin and BiP depends on their location. “It has been observed that calreticulin is often presented on the plasma membrane of tumour cells,” Eggleton explained.
On the plasma membrane, it can be exploited to act as an immunogen to alert the immune system. However, extracellularly, in solution outside the plasma membrane, it has little therapeutic value. because it can bind to immune cells directly and prevent them from recognising the tumour cell. “So, it’s important to keep the protein on the tumour cell surface and not get released if you want cytotoxic immune cells to target cancer cell for elimination.”
- Re-Educating the Immune System: a ‘Brave New World’ in Immunology
- Insights in Autoimmunity and Immunotherapy
Eggleton recalled how often immune-oncologists have described cell surface BiP is an oncogenic marker of various cancers, but believes this is simply a reflection of this ubiquitous protein working to regulate the unfolded protein response that increases in cancer cells . “Sometimes BiP naturally translocates to the tumour cell surface and presents as a tumour biomarker,” he said. This indicates the cells are naturally stressed as they over proliferate. If manipulated correctly, chaperones such as calreticulin, which is a potent DAMP molecule, can be used for inducing immunogenic cell death in tumours.
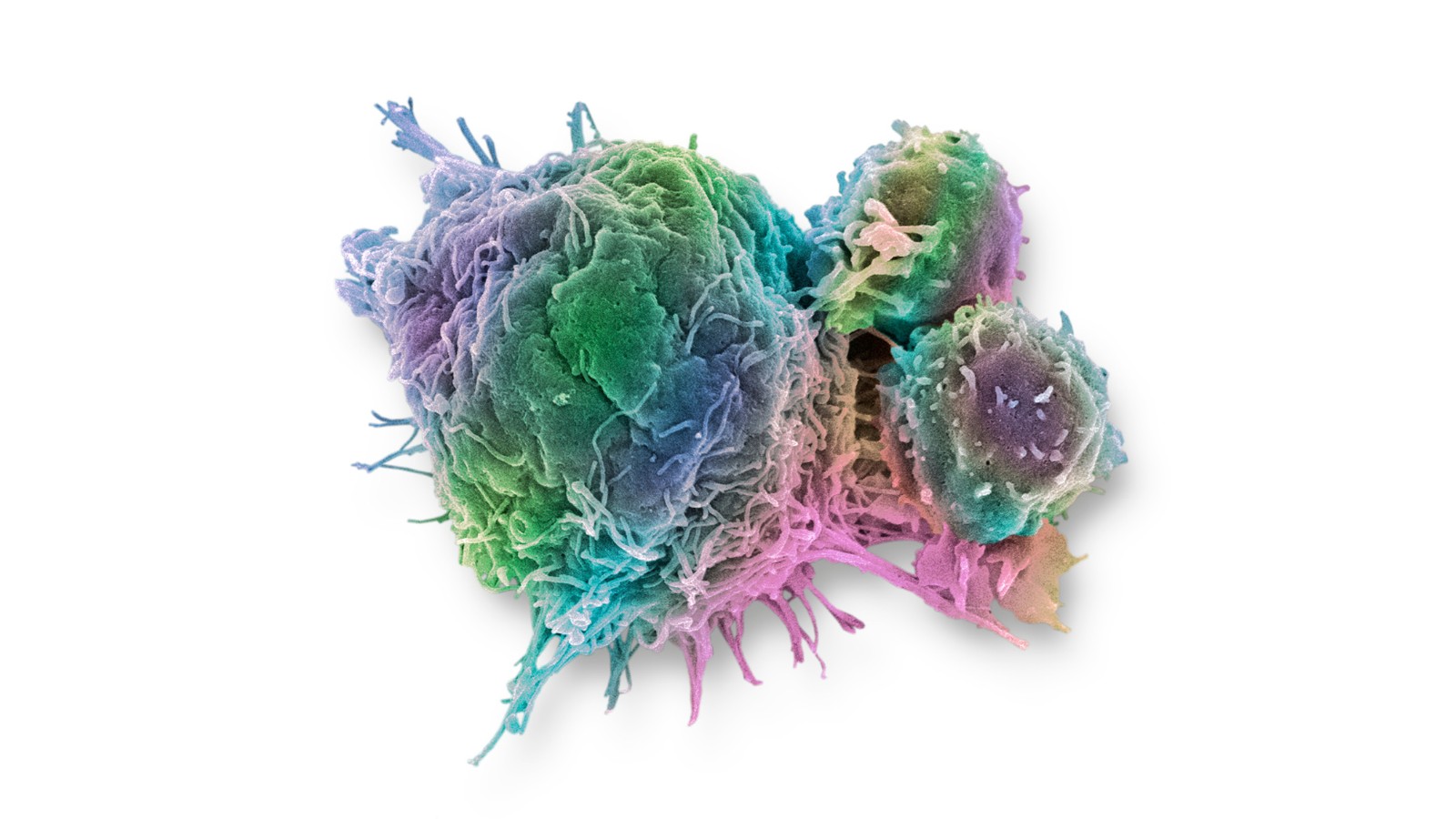
The location of BiP’s immune enhancement capacity isn’t on the cell surface; when a recombinant homologue of BiP (IRL201805) is delivered extracellularly, BiP/1805 predominantly enters macrophages and dendritic cells via different endocytic pathways. Herein, Revolo Biotherapeutics believes that BiP/1805 can be a very immune tolerogenic molecule when infused into patients. BiP/1805 initially promotes the production of tolerogenic dendritic cells which can then act in concert with T-regulatory cells to rebalance the inflammatory environment found in autoimmune tissue.
Immunogenic Cell Death of Cancer Cells – ER Stress is Key
Malignancy in the body creates profuse stress in the cells and ER such as hypoxia, oxidative stress, proliferation, and reduced amino acids. “This leads to calreticulin working overtime,” explained Eggleton. “That sends out stress signals within the ER which triggers the unfolded protein response.” This response allows proteosomes to degrade misfolded proteins to serve the survival of the cell. The translocation of calreticulin from inside the cell on to the cell surface, which has been noted in breast and ovarian cancers.
There have been many observations of chemotherapy and radiotherapy patients in which intracellular molecules are presented outside the cell such as ATP or calreticulin. Revolo’s treatment is to present DAMAGE-associated molecular pattern molecules on the surface of dying cancer cells. These molecules then interact with individual receptors on immature dendritic cells, triggering them to mature so that they can present those tumour antigens to CD4 and CD8 T cells. This releases pro-inflammatory cytokines which enhances the ability of the tumours to die.
Discover the latest developments towards achieving safe and effective NK cell-based therapy for a variety of cancer types at our Natural Killer Cell Online Symposium 2023.