Experiments Link Gut Microbiome and Graft-versus-Host Disease
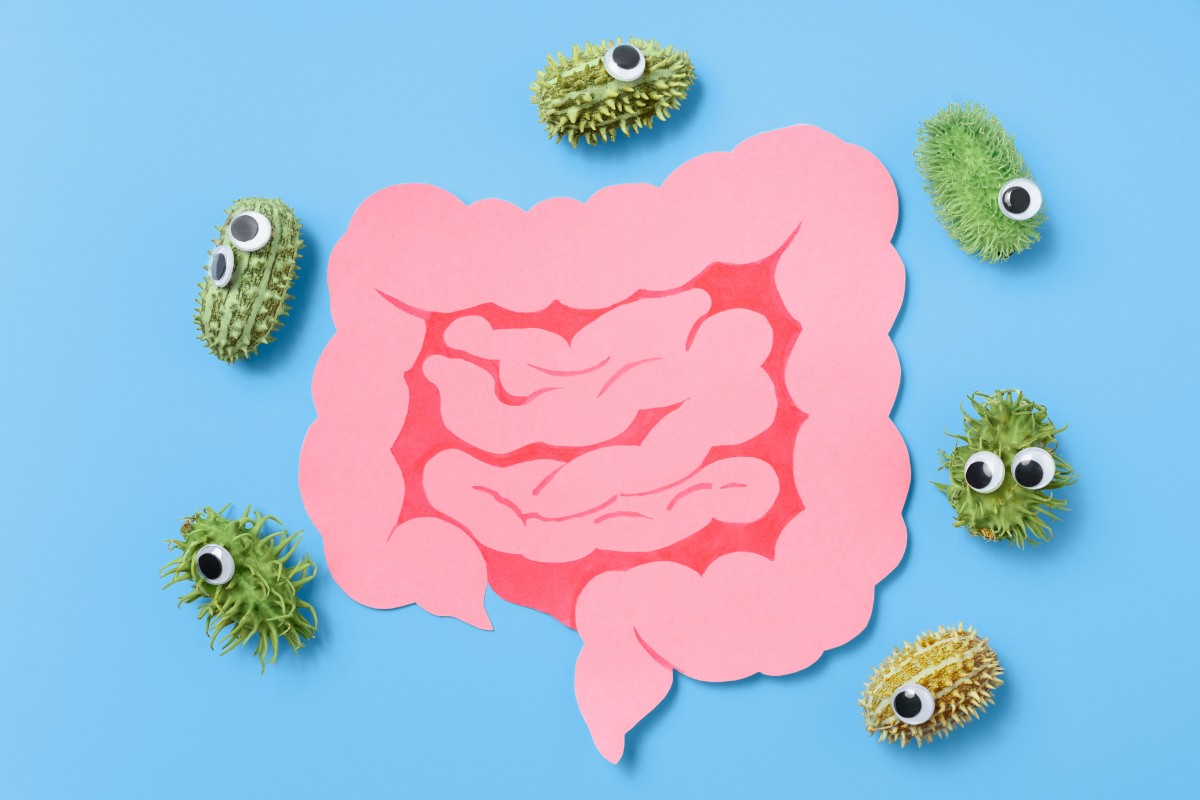
Researchers have uncovered that graft-versus-host disease from stem cell transplantation can be dependent on the types of bacteria present in patients’ gut.
The paper, published in Nature Cancer and authored by scientists at the Technical University of Munich (TUM) and the Universitätsklinikum Regensburg (UKR), found that GvHD is much more common in patients without certain bacterial families in their microbiome.
GvHD is a serious immune condition whereby transplanted immune cells attack a patients’ body after they receive a stem cell or bone marrow donation. The syndrome is treatable, but in chronic cases symptoms could last a lifetime.
Transplanting stem cells or bone marrow can be lifesaving for many patients with blood cancers, but cases of GvHD occur after roughly half of transplantations.
The study looked at stool samples from 78 patients for the two years after they received stem cell transplants. Erik Thiele Orberg led the study at the Clinic and Polyclinic for Internal Medicine III.
Orberg described their approach: “Instead of counting bacteria, we measured the quantities of certain metabolites produced by the microbes.”
These metabolites, known as immune modulatory metabolites (IMMs), can affect the efficacy of immune system. On top of these bacteria and metabolites, bacteriophage viruses in the gut microbiome can also influence immune responses.
As Elisabeth Meedt, UKR physician and the study’s lead author, explained: “This alone offers an impressive insight into the complex world of our gut microbiome.”
The study has been spotlighted by The Technical University of Munich’s news feed, which says that the collaboration between TUM and UKR will now look at modulating the gut microbiota with the hopes of curing patients.
Citing successes in mouse models, Hendrik Poeck, executive senior physician at the Clinic and Polyclinic for Internal Medicine, UKR, said: “By precisely controlling the composition of faecal microbiota transplants, the gut could be colonized with specific consortia of bacteria and bacteriophages.”
He continued: “In the coming years, we want to find out whether we can use this approach to prevent graft vs. host reactions as well as relapses.”