Cancer Vaccines: Analysing the Resurgence

The emerging development of cancer vaccines is an exciting branch of immuno-oncology. Vaccination against tumours is achieved by having the immune system recognise cancer-associated antigens to help fight cancer. Immuno 2023 featured a panel of experts discussing analysing the resurgence of this territory, its past attempts, and up-and-coming strategies.
Colleen Winstead is Director of Immunology at biotech startup Epitopea which develops mRNA LNP-based immunotherapies. Joining her was Livija Deban, Chief Scientific Officer at Prokarium, a company [re]engineering evolution into a synthetic biology platform for novel immunotherapies. The final member of the panel was Francesca Barone, Chief Scientific Officer at Candel Therapeutics. Candel uses viral immunotherapies in order to vaccinate against tumours.
- Evaxion Biotech Announce New Source of Immunotherapeutic Targets via AI Platform
- Experts Discuss Developing Oncolytic Virus Immunotherapy
- Three Leading Perspectives on Biomarker Diagnostic Discovery in Immuno-oncology
What is the Definition of Cancer Vaccines?
The panel kicked off with a fundamental question of the discussion: what is the definition of a cancer vaccine? Barone said that this was a very challenging question without a simple answer. She added that this discussion centres around therapeutic vaccination rather than prophylaxis.
“Vaccination is also not simply about delivering a tumour specific antigen – it can be broader than this and includes different modalities,” she said. Candel’s approach is to use viruses to induce cell death and the release of a multitude of antigens to activate immune cells. “It’s an important concept that you can deliver these modalities directly to the tumour, particularly to produce a systemic response.”
Another approach uses mRNA LNP vaccines: this is the technique that Winstead is interested in. “The origin of our startup is in identifying those targets that provide the most therapeutic efficacy for vaccination,” she explained. These targets are generally cancer-specific and are able to generate a very productive immune response. Winstead too said that systemic vaccination was important in order to provoke an immune response that targets the tumour.
Prokarium's modality encompasses the direct targeting of specific antigens and broader immune stimulation. Deban said that their salmonella-based therapy can induce immunogenic cell death and the release of antigens from tumour cells. They can also engineer the salmonella to deliver antigens, neo antigens, and other molecules that drive the desired immune response. In the context of cancer vaccines, it is important to guide the immune response in the right direction and to make sure that it is not overwhelmed by the suppressive tumour microenvironment.
Reasons For Past Failings
In analysing the resurgence of any modality, it is also critical to take a look back at past attempts that were perhaps not so successful. The panel next considered what the reasons for past failings were and how researchers can learn from these digressions toward a more efficacious model. This is a topic with many different interpretations, and each of our panellists gave their viewpoint:
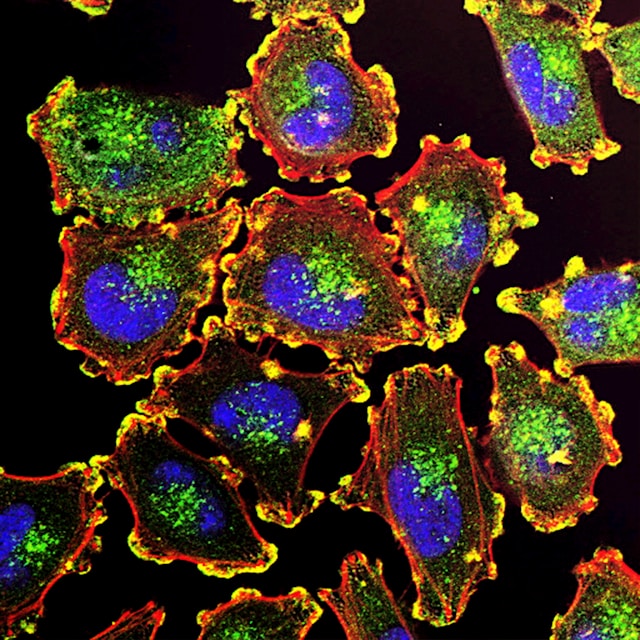
With regard to the tumour microenvironment, the absence of the right cells in the area of vaccination, or the inability of the right cells to migrate to the tumour is a worry for Deban.
Barone is focused on the ability of the immune system to recognise the right clones of tumours. One of the main problems here is that tumours can be very smart. Creating an immune response against a specific clone may end up with it downregulating a specific antigen through clonal escape – this is often how metastases form.
Tumours can mutate to elude the immune system, and so for Winstead, finding the right targets to vaccinate against can be a huge challenge. She said that the field of neoantigen vaccination is still very broad with some major issues. “If you design a vaccine and you don’t have any means to address immune escape, that’s an issue that will result in failure.” Here, Winstead is focussed on finding the right ways to solve this issue.
Will the Next Generation of Cancer Vaccines Lead to Better Clinical Outcomes?
From the viewpoint of an mRNA LNP focused company, Winstead commented that the recent success of that field had ignited some interest in using the technology to drive cancer vaccines. Furthermore, advancements in overcoming the issue of immune escape have bolstered interest in immuno-oncology more generally. This has all coincided with the technology for the development of cancer vaccines becoming cheaper, faster, and safer in the last few years.
The influence of the COVID-19 pandemic has brought to the fore public awareness around vaccination and driven its science and technology. Barone said that the science of sequencing tumours is much easier and cheaper than it ever was before. She said: “All the knowledge that we have developed through the use of checkpoint inhibitors and immunotherapy in general has enabled us to better understand how the immune system works.”
Moreover, immuno-oncologists have had to grapple with understanding the immune systems of patients that have had or are simultaneously undergoing treatments like chemotherapy and radiotherapy. Obtaining this better grasp on the tumour microenvironment has been vital for clinicians. Barone said: “We can engineer some of our vectors – our HSVs – to deliver to the liver chemokines or cytokines that can reignite the tumour microenvironment where it is needed.”
Deban agreed that since immunotherapy had become a hot topic, the field had enjoyed a reinvigoration and had seen new advances. “There are still a lot of hurdles to overcome,” she added. She offered that leveraging combinatorial approaches was a way in which to address the diversity of cancer patient populations.
Vaccines: Oncological versus Traditional Approaches
The oncological approach to developing vaccines will no doubt be very different to the way in which traditional vaccines are developed. The first contrasting feature is the timings for each, “how you induce the dynamics of an immune response in a cancer patient will be very different from a healthy individual,” said Deban. Furthermore, the COVID pandemic has accelerated the number of studies that look at regular vaccination in cancer patients.
“We also need to understand immune fitness in patients and how to boost it,” added Deban. One of Prokarium’s hypotheses is that controlled infection with an attenuated pathogen can boost the immune fitness of patients’ myeloid cells which can drive a better T cell response and systemic anti-tumour immunity.
For more insights into immuno-oncology, as well as commentaries, discussion group reports, and Q&As, sign up for our Immuno newsletter to receive monthly highlights. Are you interested in more about biomarkers in immuno-oncology? Why not come along to our next Immuno UK and Biomarkers UK conferences this year.